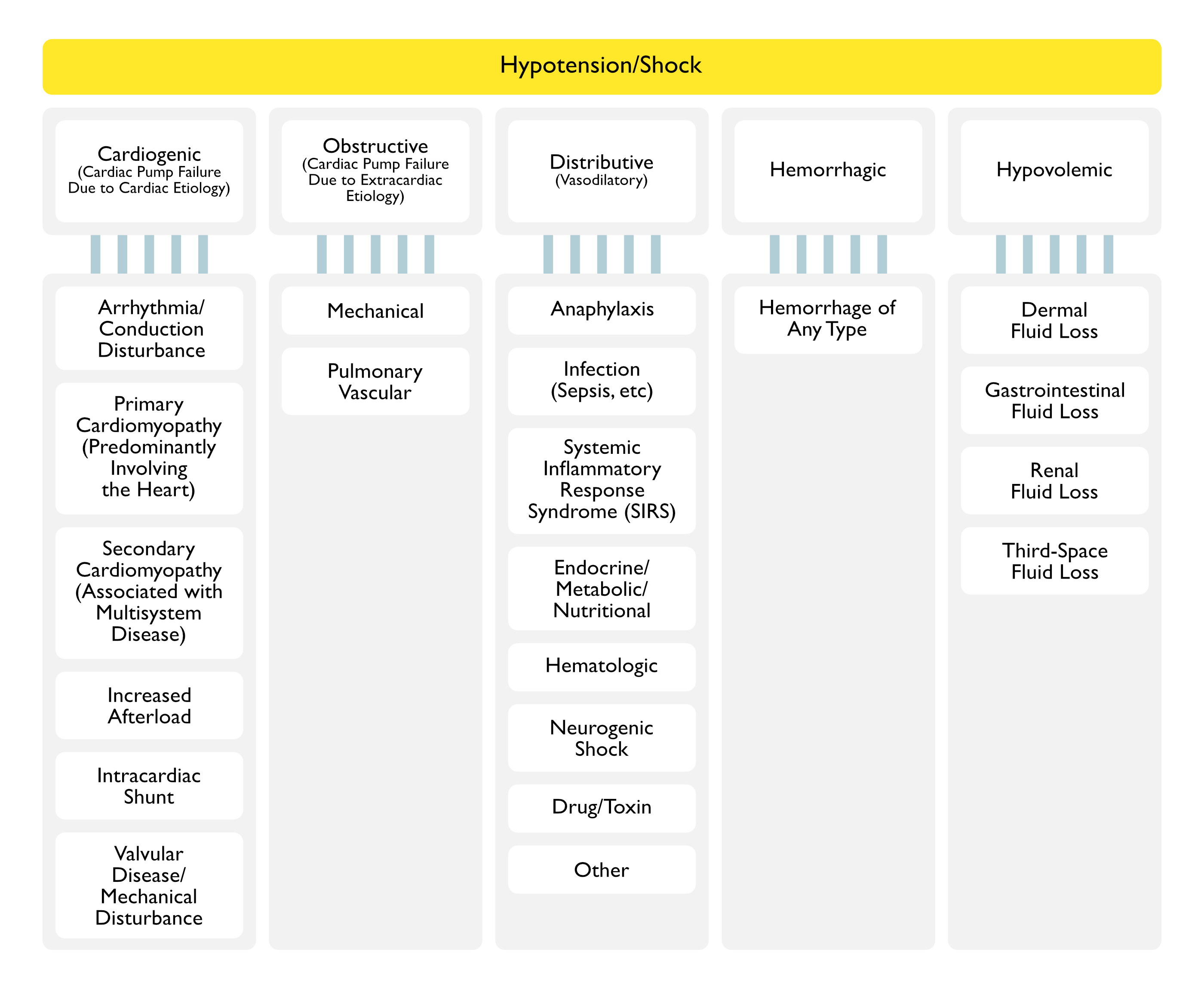
Hypotension
Etiology
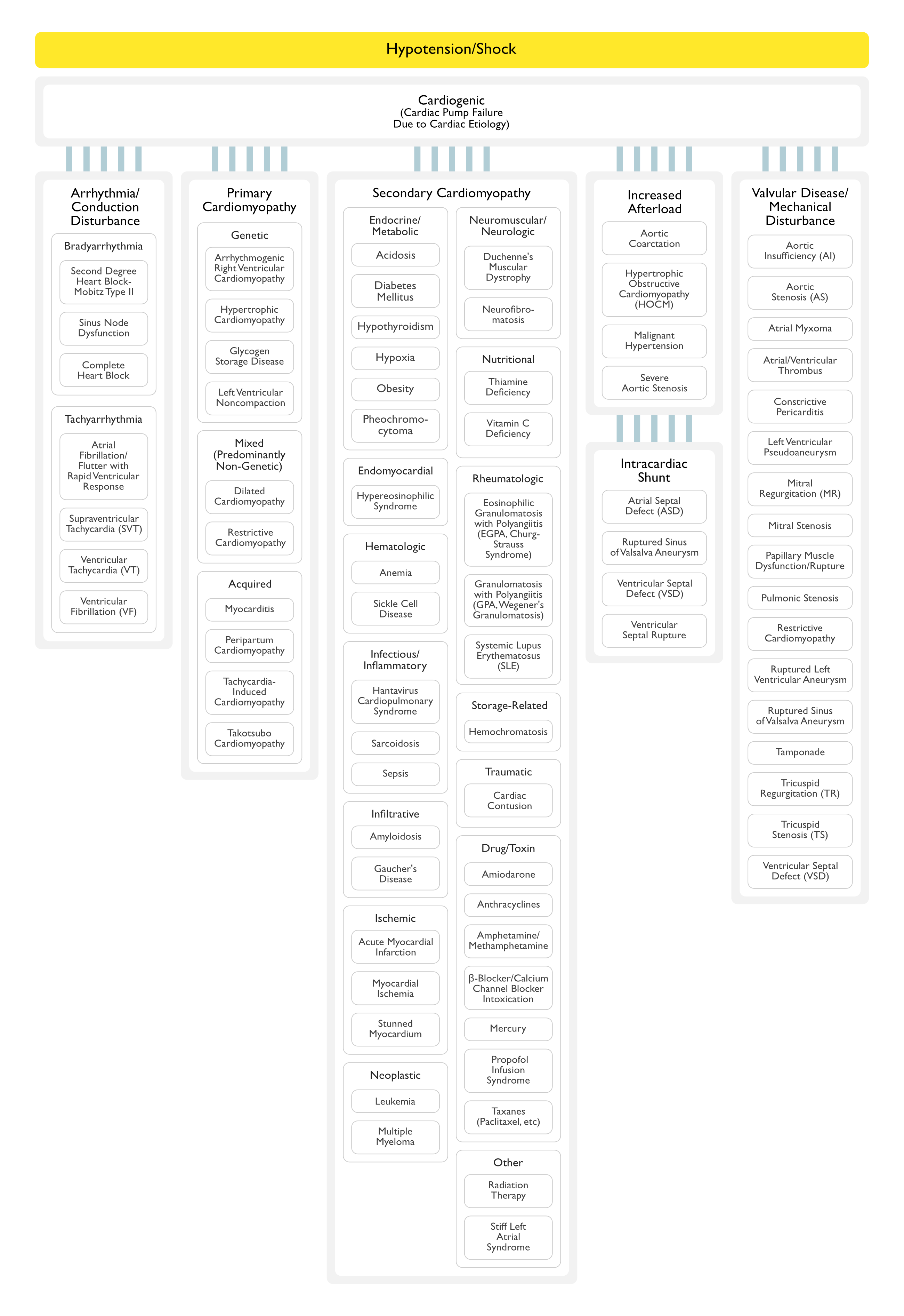
Arrhythmia/Conduction Disturbance
Bradyarrhythmia
Tachyarrythmia
Primary Cardiomyopathies (Predominantly Involving the Heart)
Genetic
Arrhythmogenic Right Ventricular Cardiomyopathy (Arrhythmogenic Right Ventricular Dysplasia) (see Arrhythmogenic Right Ventricular Cardiomyopathy )
Conduction System Disease
Glycogen Storage Diseases
Hypertrophic Cardiomyopathy
Ion Channelopathies
Brugada Syndrome
Catecholaminergic Polymorphic Ventricular Tachycardia
Idiopathic Ventricular Fibrillation
Long-QT Syndrome
Short-QT Syndrome
Left Ventricular Noncompaction
Mitochondrial Myopathies
Mixed (Predominantly Non-Genetic; Familial Disease with a Genetic Origin has been Reported in a Minority of Cases)
Dilated Cardiomyopathy: this is a heterogeneous group of disorders characaterized by ventricular dilation and decreased myocardial contractility in the absence of abnormal loading (valvular heart disease, hypertension)
Restrictive Cardiomyopathy (Non-Dilated and Non-Hypertrophied)
Acquired
Cardiomyopathy in Infants of Insulin-Dependent Diabetic Mothers
Myocarditis (Inflammatory Cardiomyopathy) (see Myocarditis )
Peripartum Cardiomyopathy
Tachycardia-Induced Cardiomyopathy
Takotsubo Cardiomyopathy (Stress Cardiomyopathy) (see Takotsubo Cardiomyopathy )
Secondary Cardiomyopathies
Cardiofacial
Lentiginosis
Noonan Syndrome
Endocrine/Metabolic
Endomyocardial
Hematologic Disease
Infectious/Inflammatory
Hantavirus Cardiopulmonary Syndrome (see Hantavirus Cardiopulmonary Syndrome ): unusually produces sepsis with a low CO and high SVR physiology
Hantavirus Genus: Sin Nombre Virus (SNV) is the most commonly associated Hantavirus in the US
Hemorrhagic Fever with Renal Syndrome (HFRS) (see Hemorrhagic Fever with Renal Syndrome )
Hantavirus Genus: Hantaan Virus, Dobrova Virus, Seoul Virus (Baltimore Rat Virus)
Sarcoidosis (see Sarcoidosis )
Sepsis-Induced Myocardial Depression (see Sepsis )
Infiltrative (Accumulation of Abnormal Substances in Extracellular Space Between Myocytes)
Amyloidosis (see Amyloidosis )
Gaucher’s Disease
Hunter’s Syndrome
Hurler’s Syndrome
Ischemic
Acute Myocardial Infarction (MI) (see Coronary Artery Disease )
Physiology: involving >40% of left ventricular myocardium or right ventricular infarction
Myocardial Ischemia
Stunned Myocardium (from Prolonged Ischemia)
Neoplasm
Neuromuscular/Neurologic
Becker Muscular Dystrophy (see Becker Muscular Dystrophy )
Chronic Progressive External Opthmoplegia (Kearns-Savre)
Duchenne Muscular Dystrophy (see Duchenne Muscular Dystrophy )
Emery-Dreifuss Muscular Dystrophy
Familial Centronuclear Myopathy
Fascioscapulohumeral Dystrophy (Landouzy-Dejerine)
Friedrich’s Ataxia
Humuloperitoneal Ataxia
Juvenile Progressive Spinal Muscular Atrophy (Kugelberg-Welander)
Limb-Girdle Muscular Dystrophy
Myotonia Atrophica (Steinert)
Myotonic Dystrophy
Neurofibromatosis (see Neurofibromatosis )
Tuberous Sclerosis (see Tuberous Sclerosis )
Nutritional
Carnitine Deficiency (see Carnitine )
Keshan’s Disease
Kwashiorkor
Niacin Deficiency (Pellagra) (see Niacin )
Selenium Deficiency (see Selenium )
Thiamine Deficiency (Beriberi) (see Thiamine )
Vitamin C Deficiency (Scurvy) (see Vitamin C )
Rheumatologic
Storage (Accumulation of Abnormal Substances Intracellularly Within Myocytes)
Traumatic
Drug/Toxin
Other
Increased Afterload
Aortic Coarctation (see Aortic Coarctation )
Epidemiology
Congenital: most cases
Acquired: few cases
Physiology
Narrowing of Descending Aorta (Typically at the Insertion of the Ductus Arteriosus Distal to the Left Subclavian Artery), Resulting in Left Ventricular Pressure Overload
Hypertrophic Obstructive Cardiomyopathy (HOCM) (see Hypertrophic Cardiomyopathy )Malignant Hypertension (see Hypertension )
Physiology
Left Ventricular Pressure Overload
Severe Aortic Stenosis (see Aortic Stenosis )
Intracardiac Shunt
Atrial Septal Defect (ASD) (see Atrial Septal Defect )
Physiology
Left-to-Right or Right-to-Left Intracardiac Shunt
Ruptured Sinus of Valsalva Aneurysm (see Sinus of Valsalva Aneurysm )
Physiology
Ruptured Sinus of Valsalva Aneurysm May Produce Aortic Insufficiency, Tricuspid Regurgitation, Left-to-Right or Right-to-Left Shunt, and/or Sudden Cardiac Death
Ventricular Septal Defect (VSD) (see Ventricular Septal Defect )
Physiology
Left-to-Right or Right-to-Left Intracardiac Shunt
Ventricular Septal Rupture (see Ventricular Septal Rupture )
Physiology
Left-to-Right or Right-to-Left Intracardiac Shunt
Valvular Heart Disease/Cardiac Mechanical Disturbance/Intracardiac Shunt
Aortic Insufficiency (AI) (see Aortic Insufficiency )
Epidemiology
Aortic Insufficiency May Be Acute in the Setting of Ascending Aortic Dissection
Physiology
Portion of Left Ventricular Stroke Volume Regurgitates Back from the Aorta into the Left Ventricle, Resulting in Increased Left Ventricular End-Diastolic Volume and Increased Left Ventricular Wall Stress
Aortic Stenosis (AS) (see Aortic Stenosis )
Physiology
Increased Left Ventricular Afterload
Atrial Myxoma (see Atrial Myxoma )
Physiology
Symptomatic Left Atrial Tumors Typically Result in Obstruction to Blood Flow, Mitral Regurgitation, and/or Systemic Embolization
Atrial Septal Defect (ASD) (see Atrial Septal Defect )
Physiology
Left-to-Right or Right-to-Left Intracardiac Shunt
Atrial Thrombus (see Intracardiac Thrombus )
Physiology
May Result in Systemic Embolization (or Less Commonly, Obstruction to Blood Flow)
Constrictive Pericarditis (see Constrictive Pericarditis )
Physiology
Early Diastolic Ventricular Filling is More Rapid Than Normal
However, Starting in Mid-Diastole, Inelastic Pericardium Results in Compression, Impairing Further Ventricular Filling and Compromising Stroke Volume
Hypertrophic Obstructive Cardiomyopathy (HOCM) (see Hypertrophic Cardiomyopathy )
Physiology
Left Ventricular Outflow Tract Obstruction
Left Ventricular Aneurysm (see Left Ventricular Aneurysm )
Physiology
Bulging of Left Ventricular Wall, Resulting in Decreased Stroke Volume
In Rare Cases Where Left Ventricular Aneurysm Rupture Occurs, Tamponade May Occur
Left Ventricular Pseudoaneurysm (see Left Ventricular Pseudoaneurysm )
Physiology
Cardiac Rupture is Contained by Adherent Pericardium or Scar Tissue (Pseudoaneurysm Contains No Endocardium or Myocardium), Resulting in Decreased Stroke Volume
In Cases Where Left Ventricular Pseudoaneurysm Rupture Occurs, Tamponade May Occur
Left Ventricular Thrombus (see Left Ventricular Thrombus )
Physiology
May Result in Systemic Embolization (or Less Commonly, Obstruction to Blood Flow)
Mitral Regurgitation (MR) (see Mitral Regurgitation )
Epidemiology
Mitral Regurgitation May Be Acute in the Setting of Myocardial Infarction-Associated Papillary Muscle Dysfunction/Rupture or Chordae Tendineae Rupture
Physiology
Decreased Effective Forward Flow
Mitral Stenosis (see Mitral Stenosis )
Physiology
Impaired Left Ventricular Filling
Pulmonic Stenosis (see Pulmonic Stenosis )
Physiology
Right Ventricular Pressure Overload
Restrictive Cardiomyopathy (see Congestive Heart Failure )
Physiology
Diastolic Dysfunction (Restricted Filling)
Ruptured Sinus of Valsalva Aneurysm (see Sinus of Valsalva Aneurysm )
Physiology
May Produce Aortic Insufficiency, Tricuspid Regurgitation, Left-to-Right or Right-to-Left Shunt, and/or Sudden Cardiac Death
Tamponade (see Tamponade )
Tricuspid Regurgitation (TR) (see Tricuspid Regurgitation )
Physiology
Right Ventricular Pressure/Volume Overload, Resulting in Right Ventricular Systolic Dysfunction
Tricuspid Stenosis (see Tricuspid Stenosis )
Physiology
Impaired Right Ventricular Filling
Ventricular Septal Defect (VSD) (see Ventricular Septal Defect )
Physiology
Left-to-Right or Right-to-Left Intracardiac Shunt
Ventricular Septal Rupture (see Ventricular Septal Rupture )
Physiology
Left-to-Right or Right-to-Left Intracardiac Shunt
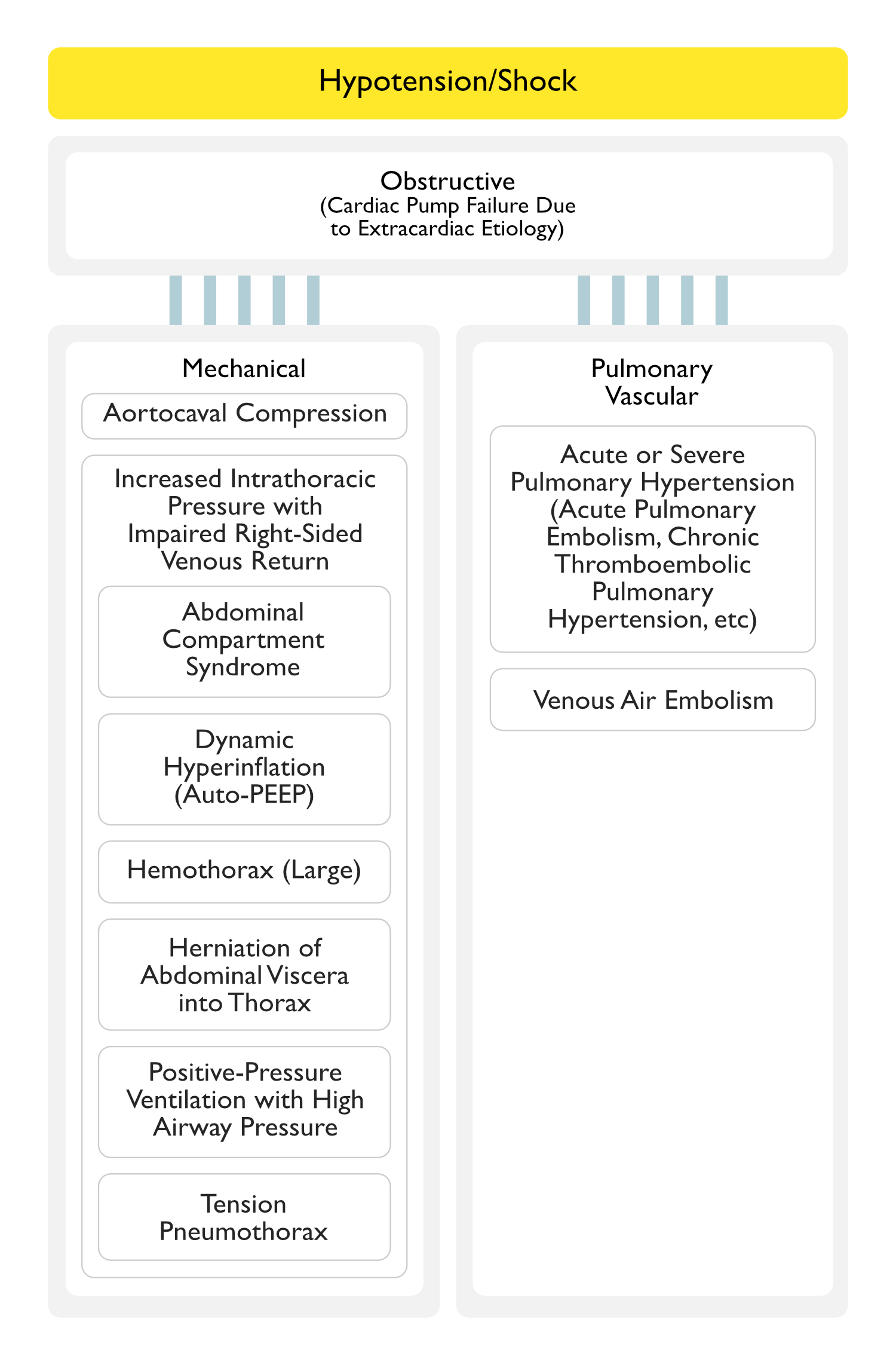
Obstructive Shock (Cardiac Pump Failure Due to an Extracardiac Etiology)
Mechanical
Aortocaval Compression (Due to Positioning or Surgical Retraction)
Physiology
Compression of Aorta, Resulting in Increased Afterload
Compression of Inferior Vena Cava, Resulting in Impaired Right-Sided Venous Return
Increased Intrathoracic Pressure (with Impaired Right-Sided Venous Return)
Abdominal Compartment Syndrome (see Abdominal Compartment Syndrome )
Physiology
Increased Intraabdominal Pressure, Resulting in Transmission with Intrathoracic Pressure, Culminating in Impaired Right-Sided Venous Return
Increased Intraabdominal Pressure, Resulting in Impaired Right-Sided Venous Return
Increased Intraabdominal Pressure, Resulting in Increased Afterload
Dynamic Hyperinflation Associated with High Positive End-Expiratory Pressure (PEEP)/Auto-PEEP (see PEEP + Auto-PEEP )
Physiology
Increased Intrathoracic Pressure, Resulting in Impaired Right-Sided Venous Return
Hemothorax (see Pleural Effusion-Hemothorax )
Physiology
Increased Intrathoracic Pressure, Resulting in Impaired Right-Sided Venous Return
Herniation of Abdominal Viscera Into Thorax
Physiology
Due to Movement of Abdominal Visceral Contents into the Thoracic Cavity, there is Increased Intrathoracic Pressure, Resulting in Impaired Right-Sided Venous Return
Positive-Pressure Ventilation with High Airway Pressures (see Acute Respiratory Distress Syndrome )
Physiology
Increased Intrathoracic Pressure, Resulting in Impaired Right-Sided Venous Return
Tension Pneumothorax (see Pneumothorax
Physiology
Increased Intrathoracic Pressure, Resulting in Impaired Right-Sided Venous Return
Pulmonary Vascular
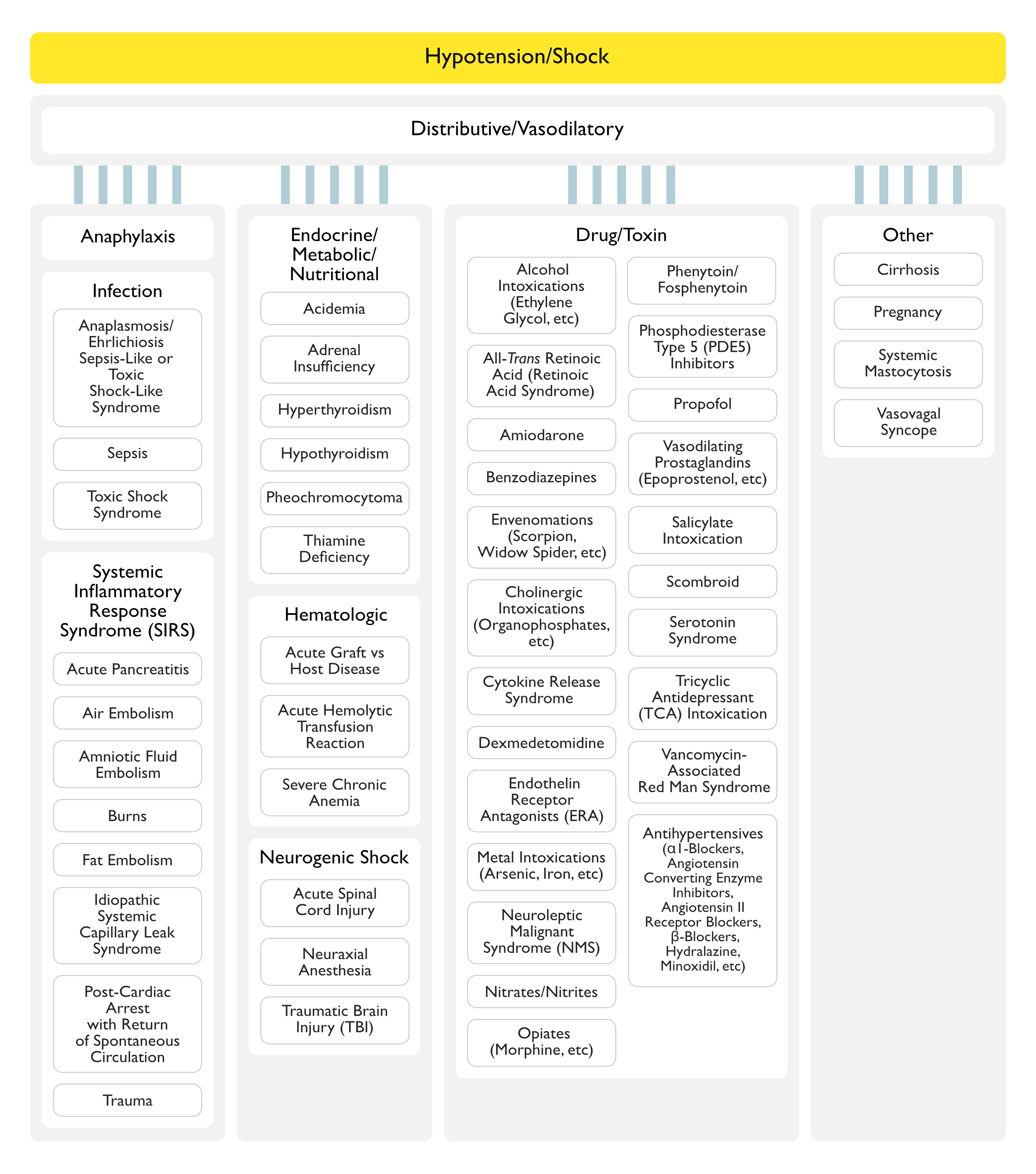
Distributive Shock (Vasodilatory Shock)
Anaphylaxis/Anaphylactic Shock
Anaphylaxis (see Anaphylaxis )
Physiology
Peripheral Vasodilation (Due to Histamine and Other Vasoactive Substances)
Infection
Anaplasmosis Sepsis-Like or Toxic Shock-Like Syndrome (see Anaplasmosis )Ehrlichiosis Sepsis-Like or Toxic Shock-Like Syndrome (see Ehrlichiosis )Sepsis/Septic Shock (see Sepsis )
Epidemiology
Sepsis is the Most Common Etiology of Distributive Sshock
Physiology
Third-Spacing of Fluids (with Decreased Intravascular Volume) and Peripheral Vasodilation
Toxic Shock Syndrome (TSS)
Systemic Inflammatory Response Syndrome (SIRS) (see Sepsis )
Endocrine/Metabolic/Nutritional Deficiency-Associated Hypotension
Acidemia
Adrenal Insufficiency (see Adrenal Insufficiency )
Hyperthyroidism (see Hyperthyroidism )
Hypocalcemia (see Hypocalcemia )
Epidemiology
Cases of Hypocalcemia-Associated Hypotension Have Been Extensively Reported (Am J Kidney Dis, 1994) [MEDLINE ] (Am J Kidney Dis, 2015) [MEDLINE ] (Hemodial Int, 2016) [MEDLINE ]
Hypocalcemia-Associated Hypotension is Most Commonly Seen When it is Rapidly Induced by Ethylenediaminetetraacetic Acid (EDTA), Transfusion of Citrated Blood, Products, or with the Use of Low Calcium Dialysate in Patients Undergoing Dialysis
Hypothyroidism/Myxedema (see Hypothyroidism )
Pheochromocytoma (see Pheochromocytoma )
Epidemiology
Clinical Patterns
Episodic Hypotension: in rare cases where the tumor secretes only epinephrine
Pattern of Rapid Cyclic Fluctuation Between Hypertension and Hypotension (Cycling Every 7-15 min): unclear mechanism
Orthostatic Hypotension: due predominantly to decreased plasma volume
Thiamine Deficiency (Beriberi) (see Thiamine )
Hematologic Disease-Associated Hypotension
Acute Spinal Cord Injury (SCI) (see Acute Spinal Cord Injury )
Physiology
Interruption of Autonomic Pathways, Resulting in Decreased Systemic Vascular Resistance and Altered Vagal Tone: probably the predominant mechanism
Myocardial Depression: may also play a role
Acute Blood Loss: may also play a role in some cases
Brain Herniation (Due to Foramen Magnum Herniation) (see Increased Intracranial Pressure )
Physiology
Compression of Brainstem and/or Upper Cervical Spinal Cord
Chronic Spinal Cord Injury (SCI) (see Acute Spinal Cord Injury )
Guillain-Barre Syndrome (GBS) (see Guillain-Barre Syndrome )
Epidemiology
Autonomic Dysfunction is Common in GBS (Occurs in Approximately 66% of Cases)
Clinical
Arrhythmias
Blood Pressure Fluctuations
Bradycardia/Tachycardia
Gastrointestinal Dysfunction
Multiple Sclerosis (see Multiple Sclerosis )
Epidemiology
Autonomic Dysfunction Can Occur
Clinical
Neuraxial (Spinal) Anesthesia (see Spinal Anesthesia )
Transverse Myelitis (see Transverse Myelitis )
Traumatic Brain Injury (TBI) (see Traumatic Brain Injury )
Drug/Toxin-Associated Hypotension
Abacavir-Hypersensitivity Reaction (see Abacavir )
Pharmacology : peripheral vasodilation
Alcohol Intoxications
Ethanol (see Ethanol )
Pharmacology: peripheral vasodilation
Ethylene Glycol Intoxication (see Ethylene Glycol )
Isopropanol Intoxication (see Isopropanol )
Methanol Intoxication (see Methanol )
Pharmacology: peripheral vasodilation
Amiodarone (Cordarone) (see Amiodarone )
Pharmacology
Peripheral Vasodilation
Negative Inotropy Can Also Occur in Patients with Preexisting Left Ventricular Dysfunction with EF <35%)
Atypical Antipsychotics (see Antipsychotic Agents )
Benzodiazepines (see Benzodiazepines )
Capsaicin (see Capsaicin )
Cholinergic Intoxication (see Cholinergic Intoxication )
Cigua Toxin Poisoning (see Cigua Toxin Poisoning )
Physiology
Dysfunction of Calcium and Sodium channels, Resulting in Peripheral Vasodilation
Cyanide Intoxication (see Cyanide )
Pharmacology
Mitochondrial Dysfunction
Clinical : hypotension occurs late in the course
Cytokine Release Syndrome (see Cytokine Release Syndrome )
Associated Agents
Alemtuzumab (Campath, MabCampath, Campath-1H, Lemtrada) (see Alemtuzumab ): anti-CD52 monoclonal antibody
Anti-Thymocyte Globulin (ATG) (see Antithymocyte Globulin )
Basiliximab (Simulect) (see Basiliximab )
Bi-Specific Antibodies in Treatment of Leukemia
Chimeric Antigen Receptor T-Cells (CAR-T) (see Chimeric Antigen Receptor T-Cells )
Haploidentical Mononuclear Cells in Treatment of Refractory Leukemia
Lenalidomide (Revlimid) (see Lenalidomide )
Muromonab-CD3 (Orthoclone OKT3) (see Muromonab-CD3 ): anti-CD3 monoclonal antibody
Oxaliplatin (Eloxatin, Oxaliplatin Medac) (see Oxaliplatin )
Rituximab (Rituxan) (see Rituximab ): chimeric monoclonal anti-CD20 antibody
Tisagenlecleucel (Kymriah) (see Tisagenlecleucel ): CAR-T (CD19-directed T-cell medication) therapy
Pharmacology
Defibrotide (Defitelio) (see Defibrotide )Dexmedetomidine (Precedex) (see Dexmedetomidine )
Differentiation Syndrome (Retinoic Acid Syndrome) (see Tretinoin )
Epidemiology
Pharmacology
Dobutamine (Dobutrex) (see Dobutamine )
Pharmacology
Myocardial β1-Adrenergic Receptor Agonist (Chronotropic/Inotropic Effects) and Vascular β2-Adrenergic/α1-Adrenergic Receptor Agonist (if Vascular β2-Adrenergic Effects exceed α1-Adrenergic Receptor Agonist Effects, Some Peripheral Vasodilation May Occur)
Eltrombopag (Promacta, Revolade)
Endothelin Receptor Antagonists (ERA’s) (see Endothelin Receptor Antagonists )
Envenomations
Estrogen (see Estrogen )
Glyphosate Ingestion (see Glyphosate )
Hemoglobinopathies
Hexoprenaline (Gynipral) (see Hexoprenaline )
Pharmacology
β2-Adrenergic Receptor Agonist
Hydrogen Sulfide Gas Inhalation (see Hydrogen Sulfide Gas )Intravenous Immunoglobulin (IVIG) (see Intravenous Immunoglobulin )L-Arginine (see L-Arginine )
Pharmacology
Nitric Oxide Induction, Resulting in Peripheral Vasodilation
Magnesium Sulfate (see Magnesium Sulfate )
Epidemiology
Hypotension May Occur with Rapid Infusion
Metal Intoxications
N-Acetylcysteine (Mucomyst, Acetadote, Fluimucil, Parvolex) (see N-Acetylcysteine )
Epidemiology
Associated with Oral Administration
Pharmacology
Nerium Oleander IntoxicationNerium Oleander )Neuroleptic Malignant Syndrome (NMS) (see Neuroleptic Malignant Syndrome )
Nitrites and Nitrates (see Nitrites and Nitrates )
Pharmacology : nitric oxide induction, resulting in Peripheral Vasodilation
Ocrelizumab (Ocrevus) (see Ocrelizumab )
Epidemiology : may occur as a component of infusion reaction
Opiates (see Opiates )
Papaverine (see Papaverine )
Phenytoin (Dilantin)Fosphenytoin (Cerebyx) (see Fosphenytoin and (see Phenytoin )
Phosphodiesterase Type 5 (PDE5) Inhibitors (see Phosphodiesterase Type 5 Inhibitors )
Pharmacology : inhibits phosphodiesterase 5/PDE5 (the enzyme which degrades cGMP), resulting in enhanced NO-mediated smooth muscle relaxation and therefore, peripheral vasodilation
Propofol (Diprivan) (see Propofol )
Prostaglandins with Vasodilatory Properties
Protamine (see Protamine )
Rasburicase (Elitek) (see Rasburicase )
Ruxolitinib (Jakafi) Withdrawal Syndrome (see Ruxolitinib )
Epidemiology : occurs 1 day-3 wks after drug withdrawal
Salicylate Intoxication (see Acetylsalicylic Acid )
Pharmacology
Clinical
Pseudosepsis with Fever, Tachypnea, Metabolic Acidosis, and Hypotension
Scombroid (see Scombroid )
Serotonin Syndrome (see Serotonin Syndrome )
Sevelamer (Renagel, Renvela) (see Sevelamer )Tetrahydrocannabinol (THC) (see Tetrahydrocannabinol )
Tetrodotoxin
Epidemiology
Associated with Ingestion of Tetrodotoxin-Contaminated Pufferfish
Physiology
Tetrodotoxin Inhibits Sodium Channels on Vascular Smooth Muscle
Theobromine (see Theobromine )
Thrombolytics (see Thrombolytics Transfusion-Associated Acute Lung Injury (TRALI) (see Transfusion-Associated Acute Lung Injury )Tricyclic Antidepressant Intoxication (see Tricyclic Antidepressants )
Vancomycin-Associated Red Man Syndrome (see Vancomycin )
Vasodilator Antihypertensives
Agents
α-Adrenergic Receptor Antagonists (see α-Adrenergic Receptor Antagonists )
Pharmacology: α2-adrenergic receptor antagonism, resulting peripheral vasodilation
α-Methyldopa (Aldomet, Aldoril, Dopamet, Dopegyt) (see α-Methyldopa )
Pharmacology: α2-adrenergic receptor agonist, resulting in peripheral vasodilation
Angiotensin Converting Enzyme (ACE) Inhibitors (see Angiotensin Converting Enzyme (ACE) Inhibitors )
Pharmacology: angiotensin converting enzyme inhibition, resulting in peripheral vasodilation
Angiotensin II Receptor Blockers (ARB) (see Angiotensin II Receptor Blockers )
Pharmacology: angiotensin II receptor inhibition, resulting in peripheral vasodilation
β-Adrenergic Receptor Antagonists (β-Blockers) (see β-Adrenergic Receptor Antagonists )
Pharmacology: β-adrenergic receptor antagonism, resulting in decreased cardiac output and peripheral vasodilation
Calcium Channel Blockers (see Calcium Channel Blockers )
Pharmacology: calcium channel antagonism, resulting in peripheral vasodilation (and additionally decreased cardiac output with some of the agents)
Clonidine (Catapres, Kapvay, Nexiclon) (see Clonidine )
Pharmacology: α2-adrenergic receptor agonism, resulting in peripheral vasodilation
Hydralazine (see Hydralazine )
Pharmacology: peripheral vasodilation
Minoxidil (see Minoxidil )
Pharmacology: direct relaxation of arteriolar smooth muscle (possibly mediated by cAMP), resulting in peripheral vasodilation
Other
Cirrhosis/End-Stage Liver Disease (see Cirrhosis )
Physiology
Characteristically Produces a High Cardiac Output (CO)/Low Systemic Vascular Resistance (SVR) State
Hepatic Veno-Occlusive Disease (see Hepatic Veno-Occlusive Disease )Hypercapnia (see Hypercapnia and Respiratory Failure )
Physiology
Hypercapnia-Induced Venodilation
Hypoxemia (see Hypoxemia and Respiratory Failure )
Physiology
Hypoxia-Induced Systemic Vasodilation (Which Attempts to Maintain Tissue Perfusion with Oxygen Delivery)
In Contrast, in the Pulmonary Circulation, Hypoxia Results in Hypoxic Pulmonary Vasoconstriction
Pregnancy (see Pregnancy )
Physiology : pregnancy increases plasma volume, increases cardiac output, increases stroke volume, increases heart rate, decreases blood pressure, and decreases SVR
Purpura Fulminans (see Purpura Fulminans )Systemic Arteriovenous Fistula (see Systemic Arteriovenous Fistula )
Types
Femoral Arteriovenous Fistula: most common type of acquired arteriovenous fistula (due to the frequency of using the femoral site for percutaneous arterial or venous access)
Hemodialysis Arteriovenous Fistula (see Hemodialysis Arteriovenous Fistula )
Clinical : high output heart failure may occur
Systemic Mastocytosis (see Systemic Mastocytosis )
Vasoplegic Syndrome (Post-Cardiac Surgery Vasodilation) (see Vasoplegic Syndrome )
Physiology
Peripheral Vasodilation Following Cardiac Surgery
Vasovagal Syncope (see Vasovagal Syncope )
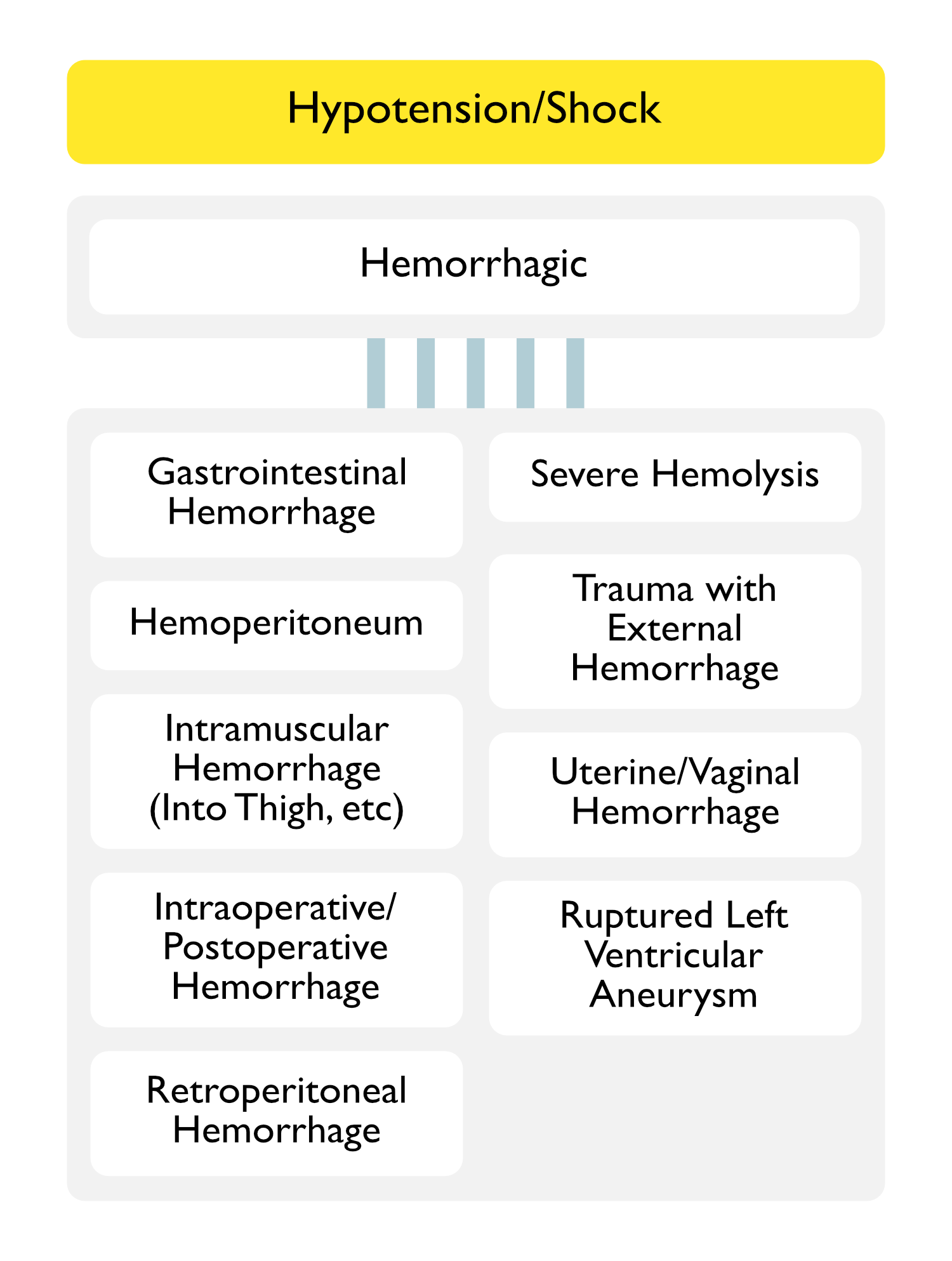
Intramuscular Hemorrhage (Into Thigh)
Intraoperative/Postoperative Hemorrhage
Trauma with External Hemorrhage
Motor Vehicle Accident (MVA) Traumatic Fall/Assault
Uterine/Vaginal Hemorrhage
Postpartum Hemorrhage
Uterine Tumor Vaginal Laceration
Other
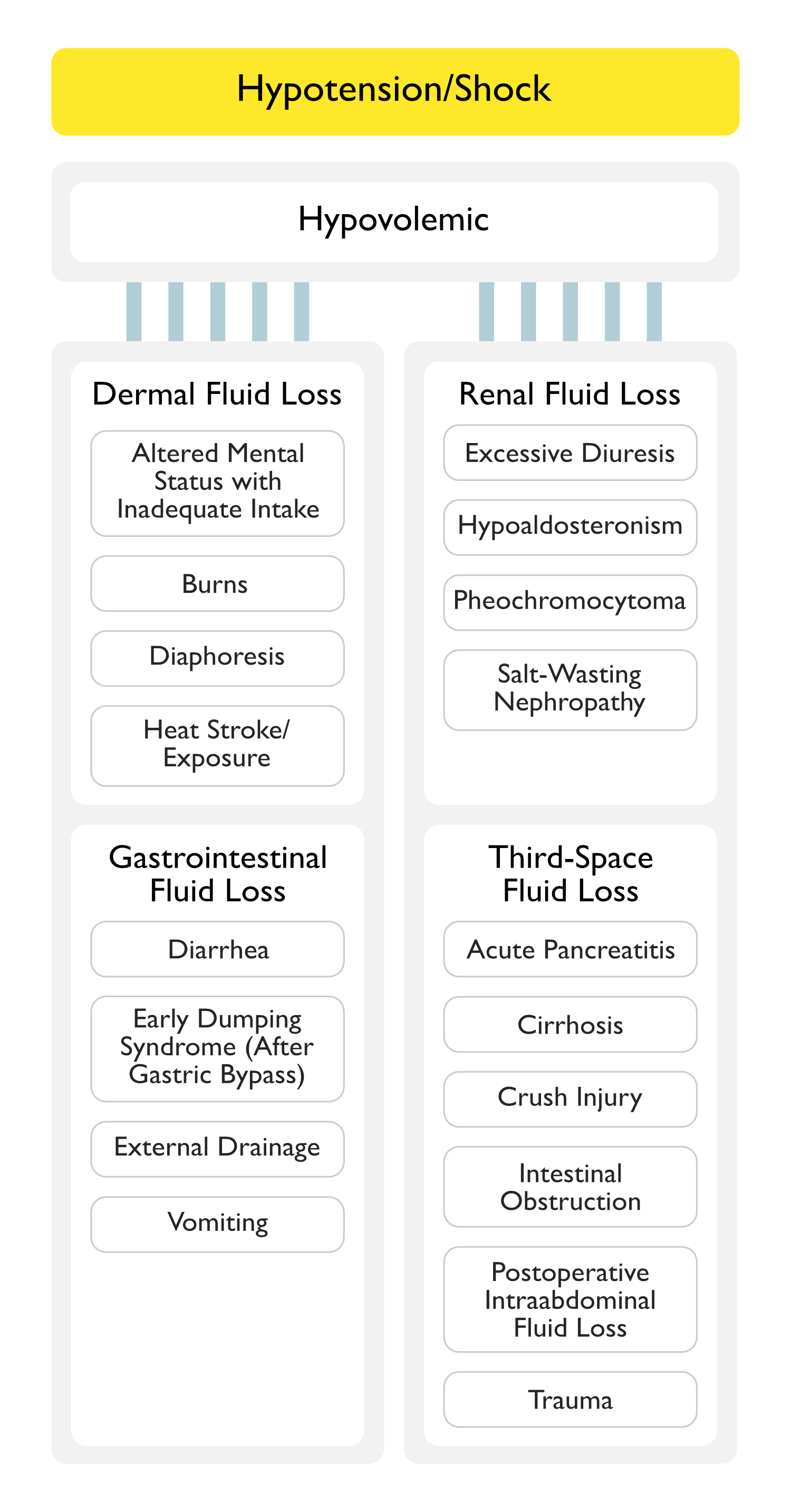
Dermal Fluid Loss
Altered Mental Status with Inadequate Fluid Intake
Burns (see Burns )Diaphoresis (see Diaphoresis )Heat Stroke/Environmental Exposure (see Heat Stroke )
Gastrointestinal Fluid Loss
Renal Fluid Loss
Excessive Diuresis Hypoaldosteronism (see Hypoaldosteronism )
Epidemiology : although aldosterone normally acts to increase sodium retention, hypoaldosteronism is not usually associated with significant sodium wasting (except in young children)
This is due to the compensatory action of other sodium-retaining stimuli (such as angiotensin II and norepinephrine)
Pheochromocytoma (see Pheochromocytoma )
Epidemiology : occurs in some casesClinical Patterns
Episodic Hypotension: in rare cases where the tumor secretes only epinephrine
Pattern of Rapid Cyclic Fluctuation Between Hypertension and Hypotension (Cycling Every 7-15 min): unclear mechanism
Orthostatic Hypotension: due predominantly to decreased plasma volume
Salt-Wasting Nephropathy
Third-Space Fluid Loss
Acute Pancreatitis (see Acute Pancreatitis )Cirhosis (see Cirrhosis )Crush Injury Intestinal Obstruction
Post-Operative Intraabdominal Fluid Loss Trauma
Diagnostic
Bedside Ultrasound
Clinical Efficacy
SHoC-ED International Randomized, Controlled Trial of Bedside Ultrasound in Undifferentiated Hypotension in the Emergency Department (Ann Emerg Med, 2018) [MEDLINE ]: n= 273
The Most Common Diagnosis in >50% of the Patients was Occult Sepsis Bedside (Point-of-Care) Ultrasound Did Not Impact the Mortality Rate, ICU or Total Length of Stay, Rate of CT Scanning, Inotrope Use, or Intravenous Fluid Administration in Undifferentiated Hypotension
Clinical Manifestations
Cardiovascular Manifestations
Neurologic Manifestations
Altered Mental Status
Fatigue (see Fatigue )Increased Intracranial Pressure (see Increased Intracranial Pressure )
Physiology : hypotension causes cerebral vasodilationClinical : potentiation of neurologic injury in traumatic brain injury (TBI), etc
Renal Manifestations
Acute Kidney Injury (AKI) (see Acute Kidney Injury )
Physiology
Acute Tubular Necrosis (ATN)
Impaired Renal Perfusion
Treatment
Vasopressors
References
Does Point-of-Care Ultrasonography Improve Clinical Outcomes in Emergency Department Patients With Undifferentiated Hypotension? An International Randomized Controlled Trial From the SHoC-ED Investigators. Ann Emerg Med. 2018 Oct;72(4):478-489. doi: 10.1016/j.annemergmed.2018.04.002 [MEDLINE ]
Property of Kenneth J. Serio, MD. Author is not responsible for errors in content, site is for information purposes only.