Epidemiology
General
- Prevalence: OSA affects about 10-17% of US population (depending on criteria used) [MEDLINE]
- Sex: 2-3x more common in adult men than adult women
- May be related to hormonal differences, differential fat deposition, craniofacial morphology, and genioglossus muscle activation
- OSA prevalence increases after menopause
- Age: OSA has 2-4x higher prevalence in elderly than in middle age
- Some studies have shown the prevalence (using AHI 5/hr) is as high as 80% in patients >71 y/o
Risk Groups
- Long-Distance Commercial Truck Drivers
- Examination of OSA Prevalence Rates in Long-Distance Commercial Truck Drivers (Sleep, 2012) [MEDLINE]: 41% of long-distance heavy vehicle drivers were likely to have sleep apnea by in-home diagnostic testing (importantly, patient self-report measures showed poor agreement with the in-home detected sleep apnea)
- 36% of drivers were overweight/50% of drivers were obese
- 49% of drivers were cigarette smokers
- Examination of OSA Prevalence Rates in Long-Distance Commercial Truck Drivers (Sleep, 2012) [MEDLINE]: 41% of long-distance heavy vehicle drivers were likely to have sleep apnea by in-home diagnostic testing (importantly, patient self-report measures showed poor agreement with the in-home detected sleep apnea)
Risk Factors/Clinical Predictors
- Acid Maltase Deficiency: OSA has been reported
- Acromegaly (see Acromegaly): OSA occurs in 60-70% of cases
- Most cases are due to anterior pituitary somatotrophin-secreting adenoma
- Best screening test is serum insulin growth factor level (GH levels can be elevated, due to increased dietary carbohydrate intake)
- Age: prevalence of OSA increases from young adulthood through the 6th-7th decade of life, then plateaus
- Chronic Lung Disease
- Asthma (see Asthma)
- Chronic Obstructive Pulmonary Disease (COPD) (see Chronic Obstructive Pulmonary Disease): 10-15% of COPD patients have OSA
- Idiopathic Pulmonary Fibrosis (IPD) (see Idiopathic Pulmonary Fibrosis)
- Congestive Heart Failure (CHF) (see Congestive Heart Failure)
- XXXXX
- Craniofacial/Upper Airway Abnormalities
- Macroglossia (see Macroglossia): due to acromegaly, etc
- End-Stage Renal Disease (ESRD) (see Chronic Kidney Disease)
- Gender: OSA is 3x more common in males, as compared to females
- Hypothyroidism (see Hypothyroidism): causes or worsens OSA
- Ischemic Cerebrovascular Accident (CVA) (see Ischemic Cerebrovascular Accident)
- Marfan Syndrome (see Marfan Syndrome)
- Menopausal/Post-Menopausal Status: xxx
- Nasal Congestion
- XXXX
- Neurologic Disease
- Alzheimer Disease (see Alzheimer Disease)
- Parkinson’s Disease (see Parkinson’s Disease)
- Obesity (see Obesity)
- Growing rates of obesity are associated with increasing OSA prevalence
- Neck Circumference >XXXXX
- Opiate Use (see Opiates)
- Polycystic Ovary Syndrome (PC) (see Polycystic Ovary Syndrome)
- Pregnancy (see Pregnancy)
- Testosterone (see Testosterone)
- Tobacco Abuse (see Tobacco) (Arch Intern Med, 1994) [MEDLINE]
Physiology
Pulmonary Hypertension (see Pulmonary Hypertension)
- Due to Hypoventilation with Resulting Hypoxia/Acidosis, Culminating in Pulmonary Vasoconstriction)
Chronic Hypoxemic, Hypercapnic Respiratory Failure (see Respiratory Failure)
- Due to Nocturnal Hypoventilation with Resulting Hypoxia/Acidosis
Diagnosis
Arterial Blood Gas (ABG) (see Arterial Blood Gas)
- Chronic Hypoventilation
- Normal A-A Gradient Hypoxemia (see Hypoxemia)
- Hypercapnia (see Hypercapnia)
Pulmonary Function Tests (PFT’s) (see Pulmonary Function Tests)
- May demonstrate restrictive pattern (if obesity is present)
Actigraphy (see Actigraphy)
- Technique: assesses sleep/wake cycle
Sleep Study (see Sleep Study)
Attended Polysomnography
- Technique
- Multi-Channel Polysomnographic Study (Including EEG Channels)
- Advantages
- EEG Channel Allows Assessment for Sleep During the Study
- Disadvantages
- More Expensive
Unattended Portable Sleep Study
- Technique
- 4-Channel Device
- Advantages
- Less Expensive
- Disadvantages
- Unattended/Portable Sleep Studies Do Not Assess for Actual Sleep: they are therefore not definitive in terms of ruling out sleep-disordered breathing
Echocardiogram (see Echocardiogram)
- May Be Useful to Assess for Concomitant Congestive Heart Failure or Pulmonary Hypertension
Clinical Manifestations
Cardiovascular Manifestations
Atrial Fibrillation (see Atrial Fibrillation)
- Epidemiology
- International Survey Study of Cardiologists Regarding Treatment of Atrial Fibrillation (Int J Cardiol Heart Vasc, 2022) [MEDLINE]: n = 863
- 33% of Respondents Referred Atrial Fibrillation Patients for Obstructive Sleep Apnea Screening
- Obstructive Sleep Apnea was Diagnosed in 48% of Referred Patients and Continuous Positive Airway Pressure (CPAP) was Prescribed for 59% of Them
- Nearly 70% of Respondents Believed Randomized Controlled Trials of Obstructive Sleep Apnea Treatment in Atrial Fibrillation Patients were Necessary and Indicated Willingness to Contribute to Such Trials
- A Majority of Cardiologists Expressed Certainty that Combined Obstructive Sleep Apnea and Atrial Fibrillation Treatment is Superior to Atrial Fibrillation Treatment Alone for Improving Atrial Fibrillation Outcomes
- However, a Minority of Cardiologists Referred Atrial Fibrillation Patients for Obstructive Sleep Apnea Testing, and While Half of Screened Atrial Fibrillation Patients Had Obstructive Sleep Apnea, CPAP was Prescribed in Little More than Half of Them, Reflecting the View that Better Clinical Trial Evidence is Required to Support This Practice
- International Survey Study of Cardiologists Regarding Treatment of Atrial Fibrillation (Int J Cardiol Heart Vasc, 2022) [MEDLINE]: n = 863
Congestive Heart Failure (CHF) (see Congestive Heart Failure)
- Epidemiology
- Obstructive Sleep Apnea Has Been Classically Associated with Group 3 Pulmonary Hypertension, Particularly When Obstructive Sleep Apnea Coexists with Either Obesity Hypoventilation Syndrome or an Alternative Etiology of Daytime Hypoxemia (Such as Chronic Lung Disease)
- Severe Hypoxemia May Also Cause Secondary Polycythemia
Hypertension (see Hypertension)
- Strong Association of Obstructive Sleep Apnea and Hypertension
- Longitudinal Sleep Heart Health Study in Adults 40-98 (2009) [MEDLINE]
- Odds Ratios for the Presence of Hypertension Increased with Increasing Apnea-Hypopnea Index (AHI) Levels
- Longitudinal Wisconsin Sleep Cohort Study in Adults 30-60 (2008) [MEDLINE]
- For even small baseline AHI elevations (1 to 5), there was an increased likelihood of developing hypertension at the 4 and 8-year time points
- 70-80% of Patients with Treatment-Resistant Hypertension Have OSA
- 30% of patients in essential hypertension clinics have OSA
- Age/male sex/AHI/BMI are all associated with hypertension, but snoring is not in OSA patients (however, in Upper Airways Resistance Syndrome, snoring is associated with hypertension)
- Longitudinal Sleep Heart Health Study in Adults 40-98 (2009) [MEDLINE]
Increased Risk of Coronary Artery Disease (CAD) (see Coronary Artery Disease)
- Epidemiology
- XXXXXXX
Increased Risk of Perioperative Cardiac Complications [MEDLINE] (Anesth Analg, 2008) [MEDLINE]
- Epidemiology
- Obstructive Sleep Apnea Increases the Risk of Perioperative Cardiovascular Complications (Br J Anaesth, 2012) [MEDLINE] (Obes Surg, 2013) [MEDLINE] (Chest, 2013) [MEDLINE] (Anesthesiology, 2014) [MEDLINE] (Sleep, 2015) [MEDLINE] (Anesth Analg, 2016) [MEDLINE] (Anesth Analg, 2018) [MEDLINE] (JAMA, 2019) [MEDLINE] (J Clin Anesth, 2020) [MEDLINE] (Eur J Anaesthesiol, 2020) [MEDLINE]
- Systematic Review and Meta-Analysis of the Impact of Obstructive Sleep Apnea on Perioperative Cardiac Complications (J Clin Anesth, 2020) [MEDLINE]: n = 3,033,814 (184,968 OSA vs 2,848,846 non-OSA) (from 22 studies)
- Obstructive Sleep Apnea is a Potential Risk Factor for Perioperative Adverse Complications in Adults Undergoing Noncardiac Surgery
- However, the Conclusions Need to Be Interpreted with Caution Due to the Nature of Included Observational Studies with Significant Heterogeneity and Low Quality of Evidence
- Clinical (Br J Anaesth, 2012) [MEDLINE] (Obes Surg, 2013) [MEDLINE] (Chest, 2013) [MEDLINE] (Anesthesiology, 2014) [MEDLINE] (Sleep, 2015) [MEDLINE] (Anesth Analg, 2016) [MEDLINE] (Anesth Analg, 2018) [MEDLINE] (JAMA, 2019) [MEDLINE] (J Clin Anesth, 2020) [MEDLINE] (Eur J Anaesthesiol, 2020) [MEDLINE]
- Atrial Fibrillation (AF) (see Atrial Fibrillation)
- Cardiac Arrest (see Cardiac Arrest)
- Congestive Heart Failure (CHF) (see Heart Failure)
- Ischemic Cerebrovascular Accident (Stroke) (see Ischemic Cerebrovascular Accident)
- Large Blood Pressure Fluctuations (see Hypertension)
- Myocardial Infarction (see Coronary Artery Disease)
- Shock
- Thromboembolism (see Deep Venous Thrombosis and Acute Pulmonary Embolism)
Endocrinologic Manifestations
Impaired Glucose Tolerance/Diabetes Mellitus (DM) (see Diabetes Mellitus)
- Epidemiology
- Impaired Glucose Tolerance and Insulin Resistance are Observed in OSA (Independent of Age and Obesity)
- Probably Due to Sleep Deprivation and Sleep-Associated Hypoxemia
- Impaired Glucose Tolerance and Insulin Resistance are Observed in OSA (Independent of Age and Obesity)
Gastrointestinal Manifestations
Increased Risk of Hepatic Steatosis/Non-Alcoholic Fatty Liver Disease (NAFLD) (see Non-Alcoholic Fatty Liver Disease)
- Epidemiology
- Study Reporting an Association Between Obstructive Sleep Apnea and Elevated Liver Function Tests/Fatty Liver (Obes Surg, 2013) [MEDLINE]
- Study Reporting an Association Between Obstructive Sleep Apnea and Hepatic Steatosis in Patients with Median BMI 34.2 (Chest, 2014) [MEDLINE]
- 61.5% of Referred Obstructive Sleep Apnea Patients Exhibited Moderate/Severe Steatosis (with 38% Manifesting Borderline/Possible Non-Alcoholic Steatohepatitis)
- Risk Factors for Hepatic Steatosis
- Nocturnal Cumulative Time Spent <90% SaO2: dose-response relationship was observed between nocturnal hypoxemia and liver injury in subset of patients with BMI >37.8
- Presence of Insulin Resistance
- Triglyceride Level
- Study Reporting an Association Between Obstructive Sleep Apnea and Hepatic Steatosis in Patients with BMI <35 (PLoS One, 2014) [MEDLINE]
- Obstructive Sleep Apnea Syndrome with Sleepiness was Strongly Associated with Non-Alcoholic Steatohepatitis and Fibrosis >1 (Independent of Known Clinical Risk Factors Such as Age, Gender, Body Mass Index (BMI), Diabetes Mellitus, and ALT Levels)
- Physiology
- Obstructive Sleep Apnea with Chronic Intermittent Hypoxemia Results in Increased Lipogenesis, Increased Triglyceride Levels, and Decreased Hepatic Beta Oxidation
Neuropsychiatric Manifestations
Excessive Daytime Somnolence (EDS) (see Excessive Daytime Somnolence)
- Epidemiology
- Common
- Diagnosis
- Epworth Sleepiness Scale
- Epworth Sleepiness Score Correlates with Risk for Motor Vehicle Accidents
- Epworth Sleepiness Scale
- Clinical
- Cognitive Impairment
- Fatigue (see Fatigue)
- Impaired Daytime Concentration
- Increased Probability of Motor Vehicle and Other Accidents
- Swedish Traffic Accident Registry Data Examining Obstructive Sleep Apnea and Risk of Motor Vehicle Accidents (Sleep, 2015) [MEDLINE]
- Obstructive Sleep Apnea Increased the Risk of Motor Vehicle Accidents with a Risk Ratio of 2.45, as Compared with Controls (p <0.001)
- Swedish Traffic Accident Registry Data Examining Obstructive Sleep Apnea and Risk of Motor Vehicle Accidents (Sleep, 2015) [MEDLINE]
Increased Risk of Cerebrovascular Accident (CVA)
- Epidemiology
- Sleep Heart Health Study (Am J Resp Crit Care Med, 2010) [MEDLINE]
- There is a Strong Adjusted Association Between Ischemic Stroke and Obstructive Apnea-Hypopnea Index in Community-Dwelling Men with Mild-Moderate Sleep Apnea
- Sleep Heart Health Study (Am J Resp Crit Care Med, 2010) [MEDLINE]
Increased Risk of Perioperative Delirium (see Delirium)
- Epidemiology
- Physiology
- Potential Mechanisms
- Compromised Regional Cerebral Blood Flow During Airway Obstruction
- Hypoxia-Associated Oxidative Stress
- Increased Serum Cortisol Levels
- Perioperative Medication
- Postoperative Pain
- Sleep Disruption
- Surgical Inflammation
- Potential Mechanisms
Morning Headache (see Headache)
- Epidemiology
- XXXXXXXX
Sleep Disruption/Frequent Arousals
- Epidemiology
- XXXXXXXX
Pulmonary Manifestations
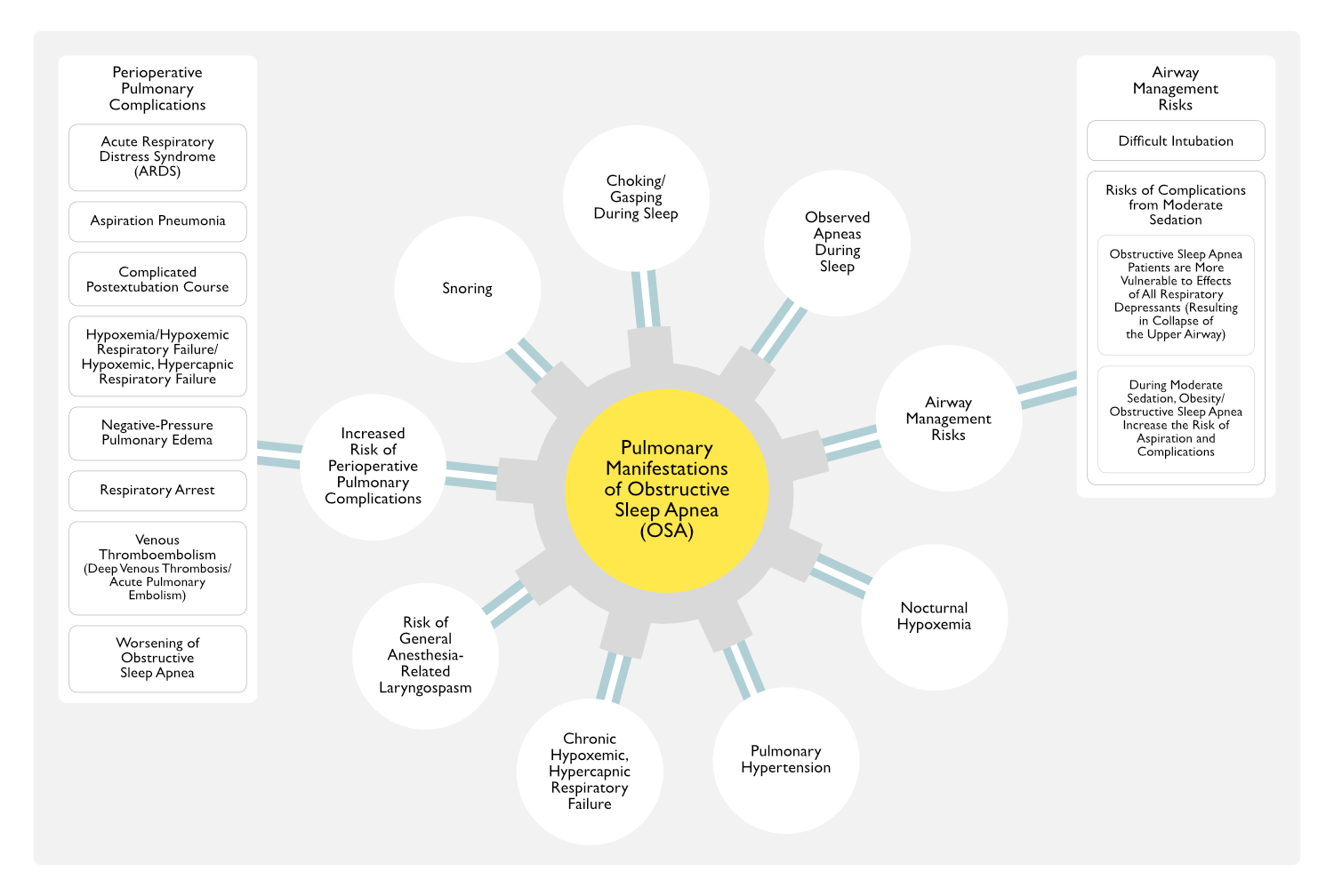
Chronic Hypoventilation/Chronic Hypoxemic, Hypercapnic Respiratory Failure (see Respiratory Failure)
- Epidemiology
- XXXXXXXXXXXXXXXXX
Increased Risk of Airway Complications (see Airway Management)
- Epidemiology
- Systematic Review and Meta-Analysis of Prospective and Retrospective Cohort Studies Examining the Effect of Obstructive Sleep Apnea on Difficult Intubation (PLoS One, 2018) [MEDLINE]
- Patients with Obstructive Sleep Apnea had a 3-4-Fold Higher Risk of Difficult Intubation or Mask Ventilation or Both, When Compared to Non-Sleep Apnea Patients
- Prospective Multicenter Observational Cohort Study of the Association Between Obstructive Sleep Apnea and Difficult Intubation Anesth Analg, 2021) [MEDLINE]
- Moderate/Severe Obstructive Sleep Apnea were Associated with Difficult Intubation
- Increasing Neck Circumference was Associated with Difficult Mask Ventilation
- A Higher STOP-Bang Score of ≥3 May Be Associated with Difficult Intubation vs STOP-Bang Score of 0-2
- Systematic Review and Meta-Analysis of Prospective and Retrospective Cohort Studies Examining the Effect of Obstructive Sleep Apnea on Difficult Intubation (PLoS One, 2018) [MEDLINE]
- Physiology
- Obstructive Sleep Apnea Patients are More Vulnerable to Respiratory Depressants (Anesth Analg, 2008) [MEDLINE]
- Alcohol (see Ethanol)
- Barbiturates (see Barbiturates)
- Benzodiazepines (see Benzodiazepines)
- General Anesthesia (see General Anesthesia)
- Opiates (see Opiates)
- Propofol (see Propofol)
- General Anesthesia Dose-Dependently Decreases Upper Airway Muscle Activity (Anesth Analg, 2008) [MEDLINE]
- Halothane Depresses Ventilation by Abolishing Peripheral Drive from Carotid Body Chemoreceptors and by Depression of Respiratory Centers in the Central Nervous System
- Halothane Also Depresses Ventilation by Suppression of the Function of Intercostal Muscles and Diaphragm
- Increasing Depth of Propofol Sedation Increases Upper Airway Muscle Collapsibility (Anesth Analg, 2008) [MEDLINE]
- Due to Combined Depression of Central Respiratory Drive to the Upper Airway Dilator Muscles and Depression of Upper Airway Reflexes
- Most Anesthetics/Opiates Used for Analgesia Can Alter the Control of Breathing by Affecting the Chemical, Metabolic or Behavioral Control of Breathing (Anesth Analg, 2008) [MEDLINE]
- Midazolam (When Administered at Sedative Doses) Can Increase Supraglottic Airway Resistance Resulting in Upper Airway Obstructive (Anesth Analg, 2008) [MEDLINE]
- Obstructive Sleep Apnea Patients are More Vulnerable to Respiratory Depressants (Anesth Analg, 2008) [MEDLINE]
- Clinical
- Difficult Intubation
- XXXXXXX
Increased Risk of General Anesthesia-Related Laryngospasm (see Laryngospasm)
- Epidemiology
- Risk Factors for General Anesthesia-Related Laryngospasm
- Airway Anomaly
- Airway Instrumentation During Light Anesthesia
- Airway Procedure (Tonsillectomy, etc) (Paediatr Anaesth, 2004) [MEDLINE]
- Vocal Cord Irritation by Inhalational Anesthetics/Secretions/Mucous/Blood
- Young Age (Acta Anaesthesiol Scand, 1984) [MEDLINE]
- Infants are at the Highest Risk
- Obstructive Sleep Apnea (OSA)
- Passive Smoke Exposure (Anesth Analg, 1996) [MEDLINE]
- Recent/Current Upper Respiratory Infection (Paediatr Anaesth, 2008) [MEDLINE] (Lancet, 2010) [MEDLINE]
- Risk Factors for General Anesthesia-Related Laryngospasm
- Clinical
- XXXXXXXXX
Increased Risk of Moderate Sedation Complications
- Epidemiology
- Obstructive Sleep Apnea Increases the Risk of Moderate Sedation Complications (Gastrointest Endosc Clin N Am, 2016) [MEDLINE]
- Obstructive Sleep Apnea May Predispose to Hypoxemia and Difficulties with Ventilation and Other Aspects of Airway Management (Anesth Essays Res, 2014) [MEDLINE]
- Procedural Sedation and Analgesia (PSA) in Patients with Obesity is Associated with a More Frequent Need for Airway Maneuvers (Such as Bag-Valve-Mask Ventilation) and More Frequent (Albeit Brief) Episodes of Hypoxemia (Gastrointest Endosc, 2011) [MEDLINE]
- However, Obesity Does Not Appear to Increase the Incidence of Serious Adverse Outcomes or Premature Termination of the Procedure
- Physiology
- Obstructive Sleep Apnea Patients are More Vulnerable to Respiratory Depressants (Anesth Analg, 2008) [MEDLINE]
- Alcohol (see Ethanol)
- Barbiturates (see Barbiturates)
- Benzodiazepines (see Benzodiazepines)
- General Anesthesia (see General Anesthesia)
- Opiates (see Opiates)
- Propofol (see Propofol)
- General Anesthesia Dose-Dependently Decreases Upper Airway Muscle Activity (Anesth Analg, 2008) [MEDLINE]
- Halothane Depresses Ventilation by Abolishing Peripheral Drive from Carotid Body Chemoreceptors and by Depression of Respiratory Centers in the Central Nervous System
- Halothane Also Depresses Ventilation by Suppression of the Function of Intercostal Muscles and Diaphragm
- Increasing Depth of Propofol Sedation Increases Upper Airway Muscle Collapsibility (Anesth Analg, 2008) [MEDLINE]
- Due to Combined Depression of Central Respiratory Drive to the Upper Airway Dilator Muscles and Depression of Upper Airway Reflexes
- Most Anesthetics/Opiates Used for Analgesia Can Alter the Control of Breathing by Affecting the Chemical, Metabolic or Behavioral Control of Breathing (Anesth Analg, 2008) [MEDLINE]
- Midazolam (When Administered at Sedative Doses) Can Increase Supraglottic Airway Resistance Resulting in Upper Airway Obstructive (Anesth Analg, 2008) [MEDLINE]
- Obstructive Sleep Apnea Patients are More Vulnerable to Respiratory Depressants (Anesth Analg, 2008) [MEDLINE]
- Clinical
- XXXXXXXX
- Management
- Adjustments in Management and Medication Dosing are Often Necessary When Providing Procedural Sedation to Adults with Obesity Due to Physiologic Changes and Associated Health Problems, Such as Obstructive Sleep Apnea and Restrictive Lung Disease (Gastrointest Endosc Clin N Am, 2016) [MEDLINE]
Increased Risk of Perioperative Pulmonary Complications (Mayo Clin Proc, 2001) [MEDLINE] (Anesth Analg, 2008) [MEDLINE]
- Epidemiology-General
- Study of the Impact of Obstructive Sleep Apnea in Patients Undergoing Hip/Knee Replacement (Mayo Clin Proc, 2001) [MEDLINE]: n = 101 patients with OSA (with 101 marched controls)
- 36 Patients Had Their Joint Replacement Before Obstructive Sleep Apnea was Diagnosed, and 65 Had Surgery After Obstructive Sleep Apnea was Diagnosed
- Of the Latter 65 Patients, Only 33 were Using CPAP at Home Preoperatively
- List of Encountered Non-Orthopedic Complications
- Acute Hypercapnia
- Arrhythmia
- Delirium
- Episodic Hypoxemia
- Myocardial Ischemia/Infarction
- Planned Intensive Care Unit Transfer
- Reintubation
- Unplanned Intensive Care Unit Transfer (In Obstructive Sleep Apnea Group: Reintubation, Hypercapnia without Reintubation, Myocardial Ischemia/Infarction, Severe Hypoxemia, Arrhythmia)
- Majority of the Cardiorespiratory/Neuropsychiatric Postoperative Complications Occurred within 72 hrs After the Joint Replacement
- Complications were Noted in 39% of Patients in the Obstructive Sleep Apnea Group vs 18% in the Control Group (P = 0.001)
- Serious Complications Occurred in 24% of Patients in the Obstructive Sleep Apnea Group vs 9% of Patients in the Control Group (P = 0.004)
- Hospital Stay was Significantly Longer for the Patients in the Obstructive Sleep Apnea Group (Mean ± SD of 6.8 ± 2.8 Days), as Compared to the Control Group (Mean 5.1 ± 4.1 Days) (P < 0.007)
- 36 Patients Had Their Joint Replacement Before Obstructive Sleep Apnea was Diagnosed, and 65 Had Surgery After Obstructive Sleep Apnea was Diagnosed
- Database Study of Pulmonary Outcomes in Patients with Obstructive Sleep Apnea After Noncardiac Surgery (Anesth Analg, 2011) [MEDLINE]: n = 6 million surgical procedures
- Patients with Obstructive Sleep Apnea Undergoing General Surgery Had Higher Rates of Intubation/Mechanical Ventilation (11% vs 6%), Aspiration Pneumonia (3% vs 2%), and Acute Respiratory Distress Syndrome (ARDS) (4% vs 2%), as Compared to Patients without Obstructive Sleep Apnea
- Patients with Obstructive Sleep Apnea Having Orthopedic Surgery Had a Similar Increase in the Risk of Complications, Although at Lower Absolute Rates, Suggesting that Risk Varies with the Type of Surgery
- Qualitative Systematic Review of Surgical Patients with Obstructive Sleep Apnea (Anesth Analg, 2016) [MEDLINE]: n = 15 studies
- Presence of Obstructive Sleep Apnea Increased the Rate of Pulmonary Complications (Odds Ratio Ranging from 1.07-4.4)
- Acute Respiratory Distress Syndrome (ARDS) (see Acute Respiratory Distress Syndrome)
- Difficult Reintubation (see Airway Management)
- Hypoxemia/Respiratory Failure (see Hypoxemia and Respiratory Failure)
- Pneumonia (see Community-Acquired Pneumonia and Hospital-Acquired Pneumonia and Ventilator-Associated Pneumonia)
- Presence of Obstructive Sleep Apnea Increased the Rate of Pulmonary Complications (Odds Ratio Ranging from 1.07-4.4)
- Prospective Cohort Study of Unrecognized Obstructive Sleep Apnea With the Occurrence of Postoperative Cardiovascular Events in Patients Undergoing Major Noncardiac Surgery (JAMA, 2019) [MEDLINE]: n = 1,364
- Obstructive Sleep Apnea was Associated with Unplanned Endotracheal Intubation or Unplanned Postoperative Noninvasive/Invasive Ventilation
- Mild OSA -> Adjusted Hazard Ratio 2.28 (95% CI: 1.04-5.03)
- Moderate OSA -> Adjusted Hazard Ratio 6.26 (95% CI: 2.85-13.75
- Severe OSA -> Adjusted Hazard Ratio 6.16 (95% CI: 2.51-15.16)
- Among At-Risk Adults Undergoing Major Noncardiac Surgery, Unrecognized Severe Obstructive Sleep Apnea was Significantly Associated with Increased Risk of 30-Day Postoperative Cardiovascular Complications
- Obstructive Sleep Apnea was Associated with Unplanned Endotracheal Intubation or Unplanned Postoperative Noninvasive/Invasive Ventilation
- Meta-Analysis of the Association Between Obstructive Sleep Apnea and Postoperative Complications (Sleep Med, 2022) [MEDLINE]: n = 46 studies
- Obstructive Sleep Apnea was Significantly Associated with Higher Risks of Postoperative Respiratory Complications (Odds Ratio = 1.91; 95% CI: 1.54-2.36) and Cardiac Complications (Odds Ratio = 1.74; 95% CI: 1.25-2.42)
- Risks Increased with Obstructive Sleep Apnea Severity
- Obstructive Sleep Apnea Also Increased the Risk of Intensive Care Unit Transfer (Odds Ratio = 1.92; 95% CI: 1.32-2.80)
- Obstructive Sleep Apnea Increased the Risk of Postoperative Delirium (Odds Ratio = 1.83; 95% CI: 1.26-2.66)
- Obstructive Sleep Apnea Prolonged Hospital Length of Stay (Weighted Mean Difference = 0.48; 95% CI: 0.15-0.82)
- Subgroup Analysis Indicated that Preoperative Diagnosis and the Use of CPAP Therapy Decrease the Risk of Postoperative Respiratory Complications (Odds Ratio = 1.87; 95% CI: 1.43-2.43) and Cardiac Complications (Odds Ratio = 1.17; 95% CI: 0.91-1.51)
- Obstructive Sleep Apnea was Significantly Associated with Higher Risks of Postoperative Respiratory Complications (Odds Ratio = 1.91; 95% CI: 1.54-2.36) and Cardiac Complications (Odds Ratio = 1.74; 95% CI: 1.25-2.42)
- The Association Between Obstructive Sleep Apnea and Perioperative Mortality Rate is Unclear (Arthroplasty, 2012) [MEDLINE] (Sleep Med, 2013) [MEDLINE] (Chest, 2013) [MEDLINE] (Obes Surg, 2013) [MEDLINE] (Anesth Analg, 2016) [MEDLINE] (JAMA, 2019) [MEDLINE] (Eur J Anaesthesiol, 2020) [MEDLINE]
- Study of the Impact of Obstructive Sleep Apnea in Patients Undergoing Hip/Knee Replacement (Mayo Clin Proc, 2001) [MEDLINE]: n = 101 patients with OSA (with 101 marched controls)
- Epidemiology-Type of Surgery
- Major Surgery, Airway Surgery, and the Use of General Anesthesia Pose Multiple Risks Which Exacerbate Airway Obstruction and Increase the Risk of Perioperative Complications in Patients with Obstructive Sleep Apnea (Sleep, 2003) [MEDLINE] (Anesthesiology, 2014) [MEDLINE]
- Depressant Effects of Anesthetics/Sedatives/Analgesics on Arousal Responses, Central Respiratory Drive, and Upper Airway Protective Reflexes
- Forced Supine Positioning
- Intense Rapid Eye Movement (REM) Sleep Rebound
- Intraluminal Upper Airway Narrowing
- Due to Post-Endotracheal Intubation Edema, Nasal Packing, Nasal Tubes, and/or Hematomas
- Rostral Fluid Shifts
- Sleep Deprivation
- Temporary Suspension of Continuous Positive Airway Pressure (CPAP) Therapy
- Due to Pain, Anxiety, Nausea, Restlessness, Presence of a Nasogastric Tube, Failure to Bring the Equipment to the Hospital, and/or Lack of Planning for Postoperative Use
- Major Surgery, Airway Surgery, and the Use of General Anesthesia Pose Multiple Risks Which Exacerbate Airway Obstruction and Increase the Risk of Perioperative Complications in Patients with Obstructive Sleep Apnea (Sleep, 2003) [MEDLINE] (Anesthesiology, 2014) [MEDLINE]
- Epidemiology-Severity of Obstructive Sleep Apnea
- Study of the Impact of Obstructive Sleep Apnea on Perioperative Complications in Bariatric Patients (Br J Anaesth, 2011) [MEDLINE]: n = 797
- In Obese Patients Preoperatively Evaluated by Polysomnogram Before Bariatric Surgery and Managed Accordingly, the Severity of Obstructive Sleep Apnea (Per the Apnea-Hypopnea Index) was Not Associated with the Rate of Perioperative Complications
- These Results Cannot Determine Whether Unrecognized and Untreated Obstructive Sleep Apnea Increases the Risk of Perioperative Complications
- Study of Postoperative Complications in Patients with Obstructive Sleep Apnea (Chest, 2012) [MEDLINE]: n = 39,771
- Patients with Obstructive Sleep Apnea are at Higher Risk of Postoperative Hypoxemia, Intensive Care Unit Transfer, and Increased Hospital Length of Stay
- Neither an Apnea-Hypopnea Index Nor the Use of Continuous Positive Airway Pressure at Home Prior to Surgery was Associated with Postoperative Complications (P = 0.3 and P = 0.75, Respectively) or Hospital Length of Stay (P = 0.97 and P = 0.21, Respectively)
- Large Retrospective Cohort Study of the Impact of Obstructive Sleep Apnea on the Outcomes of Surgical Patients (Anesthesiology, 2014) [MEDLINE]
- Pulmonary and Cardiac Perioperative Complications were Twice as Likely in Patients with Either a Known Diagnosis of Obstructive Sleep Apnea or Obstructive Sleep Apnea Diagnosed Preoperatively, as Compared to Controls without Obstructive Sleep Apnea
- Risk Increased with Increasing Severity of Obstructive Sleep Apnea
- Prospective International Cohort Study of Adult Patients Undergoing Major Noncardiac Surgery (JAMA, 2019) [MEDLINE]
- Unrecognized Severe (But Not Mild or Moderate) Obstructive Sleep Apnea was Associated with Increased 30-Day Postoperative Cardiovascular Complications
- Meta-Analysis of the Association Between Obstructive Sleep Apnea and Postoperative Complications (Sleep Med, 2022) [MEDLINE]: n = 46 studies
- Obstructive Sleep Apnea was Significantly Associated with Higher Risks of Postoperative Respiratory Complications (Odds Ratio = 1.91; 95% CI: 1.54-2.36) and Cardiac Complications (Odds Ratio = 1.74; 95% CI: 1.25-2.42)
- Risks Increased with Obstructive Sleep Apnea Severity
- Obstructive Sleep Apnea was Significantly Associated with Higher Risks of Postoperative Respiratory Complications (Odds Ratio = 1.91; 95% CI: 1.54-2.36) and Cardiac Complications (Odds Ratio = 1.74; 95% CI: 1.25-2.42)
- Study of the Impact of Obstructive Sleep Apnea on Perioperative Complications in Bariatric Patients (Br J Anaesth, 2011) [MEDLINE]: n = 797
- Epidemiology-Timing of the Diagnosis of Obstructive Sleep Apnea Relative to the Surgery
- Patients in Whom Obstructive Sleep Apnea is Newly Diagnosed at the Time of Surgery May Be at Increased Risk of Perioperative Complications, as Compared to Patients with Known Obstructive Sleep Apnea (Anesth Analg, 2017) [MEDLINE]
- Epidemiology-Requirement for the Use of Perioperative Opiates (see Opiates)
- The Requirement for Postoperative Opiates is an Important Risk Factor for the Development of Apnea/Hypoxemia in Patients with Obstructive Sleep Apnea
- Epidemiology-Comorbid Presence of Obesity-Hypoventilation Syndrome and/or Chronic Obstructive Pulmonary Disease (COPD) (see Obesity-Hypoventilation Syndrome and Chronic Obstructive Pulmonary Disease)
- As Compared to the Obstructive Sleep Apnea Alone, the Additional Presence of Obesity-Hypoventilation Syndrome or the Presence of Overlap Syndrome (Chronic Obstructive Pulmonary Disease + Obstructive Sleep Apnea) Increased the Risk of Perioperative Pulmonary and Cardiac Complications, Intensive Care Unit Transfer, and Hospital Length of Stay (Chest, 2016) [MEDLINE] (Curr Opin Anaesthesiol, 2017) [MEDLINE]
- Epidemiology-Presence of Obstructive Sleep Apnea-Related Comorbidities
- Presence of Obstructive Sleep Apnea-Related Comorbidities (Hypertension, Cardiac Arrhythmias, Coronary Artery Disease, Heart Failure) May Also Increase the Perioperative Risk (Anesth Analg, 2021) [MEDLINE]
- Clinical (Laryngoscope, 1989) [MEDLINE] (Anaesthesia, 1991) [MEDLINE] (Chest, 1995) [MEDLINE] (Anesth Analg, 1997) [MEDLINE] (Br J Anaesth, 1998) [MEDLINE] (Anesth Analg, 2002) [MEDLINE] (Sleep, 2003) [MEDLINE] (Anesth Analg, 2011) [MEDLINE] (Br J Anaesth, 2012) [MEDLINE] (Chest, 2013) [MEDLINE] (Obes Surg, 2013) [MEDLINE] (Anesth Analg, 2016) [MEDLINE]
- Acute Respiratory Distress Syndrome (ARDS) (see Acute Respiratory Distress Syndrome)
- Aspiration Pneumonia (see Aspiration Pneumonia)
- Complicated Postextubation Course
- Hypoxemia/Hypoxemic Respiratory Failure/Hypoxemic, Hypercapnic Respiratory Failure (see Hypoxemia and Respiratory Failure)
- Negative-Pressure Pulmonary Edema (see Mechanical Pulmonary Edema)
- Due to Respiration in the Setting of an Obstructed Upper Airway
- Respiratory Arrest (see Respiratory Failure)
- Venous Thromboembolism (see Deep Venous Thrombosis and Acute Pulmonary Embolism)
- Study of the Impact of Obstructive Sleep Apnea on Postoperative Complications After Revision Joint Arthoplasty (J Arthroplasty, 2012) [MEDLINE]: n = 258,455 (Nationwide Inpatient Sample)
- Obstructive Sleep Apnea was Associated with Increased In-Hospital Mortality Rate (Odds Ratio 1.9; P = 0.002), Pulmonary Embolism (Odds Ratio 2.1; P = 0.001), Wound Hematomas or Seromas (Odds Ratio 1.36; P < 0.001), and Increased Postoperative Charges ($61,044 vs $58,813; P < 0.001)
- Study of the Association of Unrecognized Obstructive Sleep Apnea With Postoperative Cardiovascular Events in Patients Undergoing Major Noncardiac Surgery (JAMA, 2019) [MEDLINE]
- Among At-Risk Adults Undergoing Major Noncardiac Surgery, Unrecognized Severe Obstructive Sleep Apnea was Significantly Associated with Increased Risk of 30-Day Postoperative Cardiovascular Complications
- Study of the Impact of Obstructive Sleep Apnea on Postoperative Complications After Revision Joint Arthoplasty (J Arthroplasty, 2012) [MEDLINE]: n = 258,455 (Nationwide Inpatient Sample)
- Worsening of Obstructive Sleep Apnea
Observed Apneas During Sleep
- Epidemiology
- XXXX
Obstructive Sleep Apnea-Chronic Obstructive Pulmonary Disease Overlap
- Epidemiology
- XXXX
- Review of the prevalence, pathogenesis and management of OSA-COPD overlap. Sleep Breath. 2022 Dec;26(4):1551-1560. doi: 10.1007/s11325-021-02540-8 [MEDLINE]
Pulmonary Hypertension/Cor Pulmonale (see Pulmonary Hypertension)
- Epidemiology
- Obstructive Sleep Apnea Has Been Classically Associated with Group 3 Pulmonary Hypertension, Particularly When Obstructive Sleep Apnea Coexists with Either Obesity Hypoventilation Syndrome or an Alternative Etiology of Daytime Hypoxemia (Such as Chronic Lung Disease)
- Severe Hypoxemia May Also Cause Secondary Polycythemia
- Pulmonary hypertension (usually mild) occurs in 15-20% of OSA patients (usually moderate-severe OSA)
- Pulmonary hypertension is believed to be associated with nocturnal hypoxemic events (therefore, in upper airway resistance syndrome, where hypoxemic events do not occur, pulmonary HTN is absent)
- There are no clinical differences between OSA patients with and without pulmonary hypertension
- Development and validation of a nomogram for predicting obstructive sleep apnea in patients with pulmonary arterial hypertension. Nat Sci Sleep. Published online August 9, 2022. doi:10.2147/NSS.S372447 [MEDLINE]
- OSA was present in 26.7% of the PAH patients, and the prevalence did not differ significantly between male (29.7%) and female (24.3%) patients. Six variables were selected to construct the nomogram, including age, body mass index, hypertension, uric acid, glycated hemoglobin, and interleukin-6 levels
- Based on receiver operating characteristic analysis, the nomogram demonstrated favorable discrimination accuracy with an area under the curve (AUC) of 0.760 for predicting OSA, exhibiting a better predictive value in contrast to ESS (AUC = 0.528) (P < 0.001). Decision curve analysis and clinical impact curve analysis also indicated the clinical utility of the nomogram
- By establishing a comprehensive and practical nomogram, we were able to predict the presence of OSA in patients with PAH, which may facilitate the early identification of patients that benefit from further diagnostic confirmation and intervention
- Comparison of obstructive sleep apnoea prevalence and severity across WHO pulmonary hypertension groups. BMJ Open Respir Res. August 2022;9(1):e001304. doi:10.1136/bmjresp-2022-001304 [MEDLINE]
- Among the cohort of 132 patients, OSA was common in all WHO pulmonary hypertension groups but was most common and most severe in WHO group II pulmonary hypertension. Median AHI or REI in WHO group II was 12.0 events/hour compared with 2.8 in group I, 3.7 in group III, 10.0 in group IV and 6.4 in group V. Multivariable negative binomial regression showed about a twofold increase in AHI or REI in WHO group II compared with WHO group I pulmonary hypertension
- Our findings demonstrate that OSA deserves greater consideration as a treatable comorbidity that may affect pulmonary haemodynamics and quality of life in patients with pulmonary hypertension across all WHO groups
Snoring
- Epidemiology
- XXXX
Nocturnal Hypoxemia (see xxxx)
- Epidemiology
- XXXX
Renal Manifestations
Increased Risk of Perioperative Renal Complications
- Epidemiology
- Clinical (see Acute Kidney Injury)
- XXXXXXXXX
Nocturia (see Nocturia)
- Epidemiology
- XXXX
Rheumatologic Manifestations
Gout (see xxxx)
- Epidemiology
- Patients with OSA may have an increased risk of developing gout compared with patients who do not have OSA (4.9 versus 2.5 percent
- The Risk of Gout Among Patients With Sleep Apnea: A Matched Cohort Study. Arthritis Rheumatol. 2019;71(1):154 [MEDLINE]
- Patients with OSA may have an increased risk of developing gout compared with patients who do not have OSA (4.9 versus 2.5 percent
Other Manifestations
Decreased Quality of Life (NEJM, 1993) [MEDLINE]
- xxx
Increased Risk of Other Perioperative Complications
- Increased Hospital Length of Stay
- Meta-Analysis of Impact of Obstructive Sleep Apnea on Perioperative Outcomes (Mayo Clin Proc, 2001) [MEDLINE] (Br J Anaesth, 2012) [MEDLINE]
- The Incidence of Postoperative Hypoxemia, Respiratory Failure, Postoperative Cardiac Events, and Intensive Care Unit Transfer was Higher in Patients with Obstructive Sleep Apnea
- Meta-Analysis of Impact of Obstructive Sleep Apnea on Perioperative Outcomes (Mayo Clin Proc, 2001) [MEDLINE] (Br J Anaesth, 2012) [MEDLINE]
- Increased Risk of Intensive Care Unit Transfer
- Meta-Analysis of Impact of Obstructive Sleep Apnea on Perioperative Outcomes (Br J Anaesth, 2012) [MEDLINE]
- The Incidence of Postoperative Hypoxemia, Respiratory Failure, Postoperative Cardiac Events, and Intensive Care Unit Transfer was Higher in Patients with Obstructive Sleep Apnea
- Meta-Analysis of Impact of Obstructive Sleep Apnea on Perioperative Outcomes (Br J Anaesth, 2012) [MEDLINE]
- Increased Risk of Postoperative Hematoma/Seroma
- Study of the Impact of Obstructive Sleep Apnea on Postoperative Complications After Revision Joint Arthoplasty (J Arthroplasty, 2012) [MEDLINE]: n = 258,455 (Nationwide Inpatient Sample)
- Obstructive Sleep Apnea was Associated with Increased In-Hospital Mortality Rate (Odds Ratio 1.9; P = 0.002), Pulmonary Embolism (Odds Ratio 2.1; P = 0.001), Wound Hematomas or Seromas (Odds Ratio 1.36; P < 0.001), and Increased Postoperative Charges ($61,044 vs $58,813; P < 0.001)
- Study of the Impact of Obstructive Sleep Apnea on Postoperative Complications After Revision Joint Arthoplasty (J Arthroplasty, 2012) [MEDLINE]: n = 258,455 (Nationwide Inpatient Sample)
Treatment
General Management
- Avoid Sedatives: as sedatives can increase the number of apneas in OSA
- Treatment of Underlying Acromegaly (see Acromegaly)
- Surgical Resection of Pituitary Adenoma or Octreotide Both Improve OSA
Weight Loss for Obesity (see Obesity)
Means
- Weight Loss
- Bariatric Surgery
- Bariatric Surgery Improves Sleep-Disordered Breathing, But Does Not Usually Result in Resolution of Obstructive Sleep Apnea
Clinical Efficacy
- Randomized Trial of Multimodal Telemonitoring for Weight Reduction in Sleep Apnea Patients (Chest, 2022) [MEDLINE]: n = 168
- ≥3% Body Weight Reduction Occurred in 33/84 (39.3%) and 21/84 (25.0%) Participants in the Multimodal- Telemonitoring and Usual CPAP Telemonitoring Groups, Respectively (p = 0.047)
- While No Significant Differences were Found Between the Two Groups in the Change in Office and Home Blood Pressure, Daily Step Counts During the Study Period were Significantly Higher in the Multimodal Telemonitoring Group than in the Usual CPAP Telemonitoring Group (4,767 (2,864-6,617) vs 3,592 (2,117-5,383) Per Day, p = 0.02)
- Multimodal Telemonitoring May Enhance Body Weight Eduction Efforts in Patients with Obstructive Sleep Apnea and Obesity
Transtracheal Oxygen (see Oxygen)
- Decreases hypoxemia and AHI (possibly due to delivery of oxygen below site of obstruction with increase in mean airway pressure and improved hypoxemia)
Positive Airway Pressure (PAP)
Modalities
- Continuous Positive Airway Pressure (CPAP) (se Continuous Positive Airway Pressure)
- Bilevel Positive Airway Pressure (BPAP) (see Bilevel Positive Airway Pressure)
- Expiratory Positive Airway Pressure (EPAP): Provent
Technique of CPAP/BPAP Titration (American Academy of Sleep Medicine, Guidelines, 2008) (J Clin Sleep Med, 2008) [MEDLINE]
- CPAP (or IPAP and/or EPAP for BPAP) Should Be Increased Until Respiratory Events are Eliminated: oxygen desaturations without associated obstructive respiratory events should not be considered in the decision to increase CPAP in adult patients
- Apneas
- Hypopneas
- Respiratory Effort-Related Arousals (RERA’s)
- Snoring
- Starting CPAP Should Be 4 cm H2O in Adults: higher starting CPAP may be used in patient with elevated BMI or for retitration studies
- Higher BMI Has Been Demonstrated to be Associated with Higher CPAP Pressures to Abolish Apneas
- CPAP Should Be Increased By at Least 1 cm H2O No More Often than q5 min
- Increase in CPAP Pressures to Target Respiratory Events
- CPAP Should Be Increased if at Least 2 Obstructive Apneas are Observed for Patients >12 y/o
- CPAP Should Be Increased if at Least 3 Hypopneas are Observed for Patients >12 y/o
- CPAP Should Be Increased if at Least 5 RERA’s are Observed for Patients >12 y/o
- CPAP Should Be Increased if at Least 3 min of Loud or Unambiguous Snoring is Observed for Patients >12 y/o
- “Exploration” of CPAP Above the Pressure at Which Respiratory Events are Controlled Should Not Exceed 5 cm H2O
- Maximum CPAP Should Be 20 cm H2O in Patients >12 y/o
- “Down” Titration of CPAP
- If Patient Awakens and Complains that Pressure is Too High, CPAP Should Be Restarted at a Lower Pressure Which Patient Finds Comfortable
- Down Titration May Be Considered, But is Not Required: due to a “hysteresis” phenomenon, during upward titration, the pressure level at which flow limitation disappears is 2-5 cm H2O higher than the pressure level at which it reappears during downward titration
- Split-Night Titration Study: same protocol should be used as for full-night titration study
- Split-Night Study is Comparable to Full-Night Titration Study, in Most Cases: except that pressures determined from split-night studies may be lower for patients with mild-to-moderate OSA who may not manifest the maximal severity of their condition during the first portion of the night
- Switch to BPAP
- If Patient is Uncomfortable/Intolerant of CPAP or if There are Continued Obstructive Respiratory Events at CPAP 15 cm H2O During a Titration Study, BPAP May Be Tried
- Use of BPAP
- Starting BPAP Pressures Should Be 8/4 in Adult Patients
- Minimum EPAP should be 4 cm H2O or the level of CPAP pressure at which obstructive events were eliminated
- Higher starting IPAP/EPAP may be used in patient with elevated BMI or for retitration studies
- IPAP and/or EPAP (Depending on Type of Obstructive Respiratory Evente) Should Be Increased By at Least 1 cm H2O in Both IPAP and EPAP No More Often than q5 min
- Maximum IPAP Should Be 30 cm H2O in Patients >12 y/o: IPAP exceeding 30 cm H2O increases the risk of barotrauma and other morbidities
- Minimum IPAP-EPAP Differential Should Be 4 cm H2O
- Maximum IPAP-EPAP Differential Should Be 10 cm H2O
- Starting BPAP Pressures Should Be 8/4 in Adult Patients
- Increase in BPAP Pressures to Target Respiratory Events
- IPAP and EPAP Should be Increased if at Least 2 Obstructive Apnea are Observed for Patients ≥12 y/o
- IPAP Should be Increased if at Least 3 Hyopneas are Observed for Patients ≥12 y/o
- IPAP Should be Increased if at Least 5 RERA’s are Observed for Patients ≥12 y/o
- IPAP Should be Increased if at Least 3 min of Loud or Unambiguous Snoring is Observed for Patients >12 y/o
- “Exploration” of IPAP Above the Pressure at Which Respiratory Events are Controlled Should Not Exceed 5 cm H2O
- “Down” Titration of BPAP
- If Patient Awakens and Complains that Pressure is Too High, IPAP Should Be Restarted at a Lower Pressure Which Patient Finds Comfortable
- Decrease in IPAP or Setting BPAP in Spontaneous-Timed (ST) Mode with Backup Rate May Be Helpful if Treatment-Emergent Central Sleep Apneas Complex Sleep Apneas) Develop
- Down Titration May Be Considered, But is Not Required:
- Quality of Titration
- “Optimal” Titration: decrease in RDI to <5/hr for at least 15 min duration and should include supine REM sleep at the selected pressure that is not continually interrupted by spontaneous arousals or awakenings
- “Good” Titration: decrease in RDI to ≤10/hr (or by 50% if baseline RDI was <15/hr) and should include supine REM sleep at the selected pressure that is not continually interrupted by spontaneous arousals or awakenings
- “Adequate” Titration: one which does not decrease RDI to ≤10/hr but does decrease RDI by 75% from baseline (especially in severe OSA) or if “optimal” or “good” criteria are met but supine REM sleep did not occur at the selected pressure
- Leak Management: mask fit or readjustment should be performed when any unintentional leak is observed
- Intentional Leak: controlled leak from the port on mask interfaces that washes out CO2 and prevents rebreathing
- Mouth Leak: pressurized air escaping via the mouth when a nasal mask is used
- Mask Leak: pressurized air escaping between the mask and the face when a nasal mask or full-face mask is used
- Supplemental Oxygen (see Oxygen)
- Supplemental Oxygen Should Be Added to PAP Titration When Supine SpO2 on Room Air is ≤88%: start at 1L/min and titrate up to target a SpO2 88-94%
- Supplemental Oxygen May Be Added to PAP Titration When Supine SpO2 is ≤88% for ≥5 min in the Absence of Obstructive Respiratory Events: start at 1L/min and titrate up to target a SpO2 88-94%
- Adaptive Servo Ventilation (ASV) (see Adaptive Servo Ventilation)
- ASV May Be Considered if Patient is Observed to Have Cheyne-Stokes Respiration or if Treatment-Emergent Central Sleep Anea (Complex Sleep Apnea) During the Titration Study is Not Eliminated by Down Titration of Pressure
Clinical Benefits of Continuous Positive Airway Pressure (CPAP)
- CPAP is Highly Effective in the Treatment of OSA
- However, many patients may not be adherent (for various reasons)
- CPAP Has Beneficial Effects on Atrial Fibrillation (AF) (see Atrial Fibrillation)
- Use of CPAP (>4 hrs/nt) in OSA Patients with AF Has Been Shown to Decrease Recurrence of Atrial Fibrillation After Cardioversion (42% Recurrence Rate vs. 82% Recurrence Rate)
- Effect of CPAP May Be Related to Effects of OSA on Nocturnal Hypoxemia, Hypercapnia, Sympathetic Drive, and Changes in Intrathoracic Pressure
- Use of CPAP (>4 hrs/nt) in OSA Patients with AF Has Been Shown to Decrease Recurrence of Atrial Fibrillation After Cardioversion (42% Recurrence Rate vs. 82% Recurrence Rate)
Hunt TE, Traaen GM, Aakerøy L, et al. Effect of continuous positive airway pressure therapy on recurrence of atrial fibrillation after pulmonary vein isolation in patients with obstructive sleep apnea: A randomized controlled trial. Heart Rhythm. Published online June 16, 2022. doi:10.1016/j.hrthm.2022.06.016
- CPAP Has Beneficial Effects on Pulmonary Hypertension (see Pulmonary Hypertension)
- CPAP Decreases Pulmonary Artery Pressure
- Improvement in Pulmonary Artery Pressure Occurs Independent of Changes in Hypoxemia, Suggesting that Pulmonary Artery Pressure Changes are Related to Changes in Endothelial Function, Rather than Merely a Reversal of Hypoxic Pulmonary Arterial Vasoconstriction
- CPAP Has Beneficial Effects on Systemic Hypertension (see Hypertension)
- Systematic Review/Meta-Analysis of Effects of Positive Pressure Therapy on Hypertension Associated with OSA (J Clin Sleep Med, 2012) [MEDLINE]: positive pressure therapy results in modest, but significant, decreases in systolic and diastolic blood pressure
- However, Data Indicate that the Effects of CPAP are Less Clear in the Treatment of OSA without Sleepiness
- CPAP Has Beneficial Effects on Sleep Apnea-Related Risk of Motor Vehicle Accidents
- Swedish Traffic Accident Registry Data Examining OSA and Risk of Motor Vehicle Accidents (Sleep, 2015) [MEDLINE]
- In Patients with OSA, CPAP Use ≥4 hrs/Night Was Associated with a Decrease in the Incidence of Motor Vehicle Accidents (7.6 -> 2.5 Accidents/1,000 Drivers/yr)
- Swedish Traffic Accident Registry Data Examining OSA and Risk of Motor Vehicle Accidents (Sleep, 2015) [MEDLINE]
- CPAP Has Beneficial Effects on Post-Traumatic Stress Disorder (PTSD) (see Post-Traumatic Stress Disorder)
- Study of Effects of CPAP on PTSD in Veterans with OSA (J Clin Sleep Med, 2014) [MEDLINE]
- In Veterans with PTSD and OSA, CPAP Therapy Reduces PTSD-Associated Nightmares and Improves Overall PTSD Symptoms
- Study of Effects of CPAP on PTSD in Veterans with OSA (J Clin Sleep Med, 2014) [MEDLINE]
- CPAP Therapy Alone Does Not Result in Weight Loss (see Weight Loss)
- Effect of CPAP on Cardiometabolic Parameters in OSA (Thorax, 2012) [MEDLINE]
- CPAP Alone Does Not Lead to Weight Loss or Improvement in Insulin Sensitivity
- Effect of CPAP on Cardiometabolic Parameters in OSA (Thorax, 2012) [MEDLINE]
- CPAP Therapy Alone Does Not Result in Improvement in Depression (see Depression)
Clinical Efficacy-CPAP
- Multicenter, Randomized MERGE Trial of CPAP in Mild Obstructive Sleep Apnea (Lancet Respir Med, 2020) [MEDLINE]
- Three Month Treatment of Mild OSA with CPAP Improved Quality of Life
- ISAACC Trial of CPAP Effect on the Prevalence of Cardiovascular Events in Patients with Acute Coronary Syndrome (Lancet Respir Med, 2020) [MEDLINE]
- Among Non-Sleepy Patients with Acute Coronary Syndrome, the Presence of OSA was not associated with an increased prevalence of cardiovascular events and treatment with CPAP did not significantly reduce this prevalence
Clinical Efficacy-CPAP (with Relation to Air Pollution)
- Canadian Retrospective Community-Based Study of Impact of Air Pollution on CPAP Effectiveness (Chest, 2022) [MEDLINE]: n = 8,148
- The Median Daily Device-Derived Residual Apnea-Hypopnea Index (AHIFlow) was 1.2/hr (Interquartile Range: 0.5-2.5)
- In mixed multivariate regression analyses, an increase in air pollution was associated with a statistically significant increase in Daily Device-Derived Residual Apnea-Hypopnea Index (AHIFlow) for Most Statistical Models
- Largest Effect was for the Air Quality Health Index (AQHI): an increase in daily device-derived residual apnea-hypopnea index (AHIFlow) while comparing highest vs lowest quartiles was 0.07/hour (95% CI: 0.05-0.10)
- Conclusion
- There is a Modest but statistically significant increase in residual respiratory events on Positive Airway Pressure Therapy associated with an increase in air pollution concentrations
Autotitrating Continuous Positive Airway Pressure (CPAP) (see Continuous Positive Airway Pressure)
- Rationale: autotitrating CPAP devices may be used in lieu of an in-laboratory CPAP titration study in some patients (and insurers may deny the in-laboratory study, instead requiring that an autotitrating CPAP be used)
- Contraindications
- Lack of Respiratory Drive: since the pressure delivered is triggered by respiratory effort
- Technique
- From the Autotitration Report, it is Generally Accepted to Choose the T90 or T95 Pressure (Which is the Pressure the Patient is at or Below 90-95% of the Time)
- Due to Limitations of These Devices, Patients Need Follow-Up to Ensure that this is the Correct Setting: if symptoms persist, in-laboratory titration may be required
- Factors Which May Decrease Auto-PAP Adherence
- Air Leak: auto-PAP systems are very sensitive to air leaks
- Clinical Efficacy
- Study of Auto-PAP Therapy for OSA (Sleep, 2011) [MEDLINE]
- Air Leak was Associated with Poor Adherence with Auto-PAP
- Adherence to Auto-PAP Therapy was Strongly Correlated with Subsequent Adherence to CPAP Therapy
- Residual Sleep-Disordered Breathing During Autotitrating CPAP Therapy (Eur Resp J, 2012)MEDLINE]
- Residual OSA (AHI ≥10 Events/hr) was Observed in 24% of Patients During Autotitration: for this reason, clinicians should be aware of the limitations of auto-PAP devices
- Study of Auto-PAP Therapy for OSA (Sleep, 2011) [MEDLINE]
Expiratory Positive Airway Pressure (EPAP) (Provent)
- Indications
- Alternative Therapy for Patients with Mild/Positional Who are OSA Intolerant of CPAP and Oral Devices
- Clinical Efficacy
- Only Small Studies Demonstrate Benefit in Mild/Positional OSA
Continuous Positive Airway Pressure (CPAP) Adherence
- Chronic CPAP Adherence is Predicted by the Initial First Few Days of Use by the Patient [MEDLINE]
- Factors Which May Decrease CPAP Adherence
- Air Leak
- Nasal Dryness
- Post-Traumatic Stress Disorder (PTSD) (see Post-Traumatic Stress Disorder)
- Rhinorrhea (see Rhinorrhea)
- Measures/Factors Which May Enhance CPAP Adherence
- Cognitive Behavioral Therapy (CBT)
- Education and Early, Frequent Contact with Health Care Providers After CPAP Initiation
- Family Involvement
- Heated Humidification
- More Severe Sleep Apnea Indices
- Short Course of Eszopiclone (Lunesta) During the First 2 Weeks of CPAP Therapy (Ann Intern Med, 2009) [MEDLINE] (see Eszopiclone): improves adherence and results in Fewer patients discontinuing CPAP therapy
Complications of Continuous Positive Airway Pressure (CPAP)
- Treatment-Emergent Central Sleep Apnea (Complex Sleep Apnea) (see Central Sleep Apnea)
- History: recently added to the International Classification of Sleep Disorders, 3rd ed (Chest, 2014) [MEDLINE]
- Definition: development of central sleep apnea following the application of CPAP, dental appliance, or following tracheostomy for OSA
- These Central Events Cannot Be Attributed to Another Identifiable Comorbidity Such as Cheyne-Stokes Breathing or the Use of Opiates
- Mechanism: may be related to hypocapnia or mask leaks in some cases (J Clin Sleep Med, 2013) [MEDLINE]
- Clinical
- Usually Observed When the Patient Has Frequent Arousals from Sleep
- Occurs After the Obstructive Events are Controlled During NREM Sleep: occur mainly in the supine position
- Treatment
- May Resolve Over Time in Some Cases: should reassess patient on CPAP in 2-3 mo
- Complex Sleep Apnea Resolution Study (Sleep, 2014) [MEDLINE]: central sleep apnea improves or resolves spontaneously in approximately 66% of patients who continue on CPAP for 90 days
- Adaptive Servo Ventilation (ASV) (see Adaptive Servo Ventilation): may be useful, as it treats both obstructive and central apneas
- ASV is a form of bi-level positive airway pressure that provides variable pressure support via a servo mechanism-based assessment of the patient’s respiratory output
- When There are Hypopneas: ASV increases the pressure support (difference between expiratory PAP and inspiratory PAP)
- When There are Hyperpneas: ASV decreases the pressure support (difference between expiratory PAP and inspiratory PAP)
- When Central Sleep Apneas Occur: ASV utilizes a backup rate and the EPAP maintains airway patency
- ASV increases the mortality rate in patients with central sleep apnea in association with systolic congestive heart failure and EF <45% (NEJM, 2015) [MEDLINE]
- Bilevel Positive Airway Pressure (BPAP) with Backup Rate (see Bilevel Positive Airway Pressure)
- Avoid Using BPAP without a Backup Rate: may worsen the apnea-hypopnea index (AHI)
- May Resolve Over Time in Some Cases: should reassess patient on CPAP in 2-3 mo
Management of Residual Excessive Daytime Sleepiness (see Excessive Daytime Sleepiness)
- Confirm Compliance with CPAP
- Evaluate for Other Potential Etiologies of Daytime Sleepiness (Narcolepsy, Sleep Deprivation, Shift Work Disorder, Idiopathic Hypersomnia, etc)
- Modafinil (Alertec, Modavigil, Modiodal, Provigil, Modalert) (see Modafinil)
- Mechanism: acts as a stimulant by inhibiting dopamine and hypocretin reuptake
Implantable Upper Airway Stimulation Device (Hypoglossal Nerve Stimulator)
- Indications
- OSA with Inability to Tolerate CPAP: device increases upper airway patency (but does not correct central sleep apnea)
- Device Has Not Been Tested in Treatment Emergent Central Sleep Apnea (Complex Sleep Apnea)
- OSA with Inability to Tolerate CPAP: device increases upper airway patency (but does not correct central sleep apnea)
- Clinical Efficacy
- Drug-Induced Sleep Endoscopy as a Selection Tool for Upper Airway Stimulation (J Clin Sleep Med, 2013) [MEDLINE]
- The Absence of Palatal Complete Concentric Collapse (at the Tongue Level) During Drug-Induced Sleep Endoscopy Predicts Therapeutic Success with Implanted Upper Airway Stimulator Therapy
- STAR Trial of Hypoglossal Nerve Stimulator in Moderate-Severe OSA (NEJM, 2014) [MEDLINE]: multi-center, prospective, single group, cohort design trial (n = 126) of surgically implanted upper-airway stimulation device (from Inspire Medical Systems) in moderate-severe OSA patients intolerant of CPAP (BMI <32, no major underlying cardiopulmonary disease, no other sleep disorders, no psychiatric disease)
- Hypoglossal Nerve Stimulator Resulted in a 68% Decrease in the Apnea-Hypopnea Index at 12 mo, Less Oxygen Desaturation, and Improved Quality of Life
- Patients Used the Device for at Least Part of the Night on 86% of the Nights
- Procedure-Related Serious Adverse Events Occurred in <2% of cases (temporary tongue weakness, discomfort with stimulation, tongue soreness)
- Drug-Induced Sleep Endoscopy as a Selection Tool for Upper Airway Stimulation (J Clin Sleep Med, 2013) [MEDLINE]
Dental Appliance (Most are Mandibular Advancement Devices)
- Variety of Appliances
- There are >80 Dental Appliances Available
- Mandibular Advancement Devices: accounts for most of the available devices
- Tongue Retaining Devices: accounts for remainder of devices
- There are >80 Dental Appliances Available
- Indications: second-line therapy
- Snoring and Mild-Moderate OSA Intolerant of CPAP Therapy
- Technique: polysomnography should be performed to assess efficacy
- Clinical Efficacy
- Randomized Trial Comparing CPAP with Mandibular Advancement Device in Moderate-Severe OSA (Am J Respir Crit Care Med, 2013) [MEDLINE]
- CPAP was More Efficacious than Mandibular Advancement Device in Reducing AHI
- Compliance was Higher with Mandibular Advancement Device than with CPAP
- Neither Treatment Improved Blood Pressure
- Daytime Sleepiness, Driving Simulator Performance, and Disease-Specific Quality of Life Improved on Both Treatments by Similar Amounts
- Mandibular Advancement Device was Superior to CPAP in Terms of Improving Four General Quality of Life Domains
- Randomized Trial Comparing CPAP with Mandibular Advancement Device in Moderate-Severe OSA (Am J Respir Crit Care Med, 2013) [MEDLINE]
- Complications
- Treatment Emergent Central Sleep Apnea (Complex Sleep Apnea): refers to the development of central sleep following the application of CPAP or a dental appliance
- See Above
- Treatment Emergent Central Sleep Apnea (Complex Sleep Apnea): refers to the development of central sleep following the application of CPAP or a dental appliance
Adenotonsillectomy (see xxxx)
Clinical Efficacy
- Effective in children and infants
Maxillomandibular Advancement
Technique
- Surgery to move the upper and lower jaw forward
Clinical Efficacy
- Has Been Successful in Resolving Obstructive Sleep Apnea
Uvulopalatopharyngoplasty (UPPP) (see Uvulopalatopharyngoplasty)
Technique
- Reduction or Removal of Portions of the Soft Palate and Uvula
Clinical Efficacy
- Generally Not Successful in Resolving Obstructive Sleep Apnea
Tracheostomy (see Tracheostomy)
- Indications
- Last Resort for Severe Refractory Symptomatic OSA in Patients Who are Intolerant of CPAP Therapy
Atomoxetine and Oxybutynin (see Atomoxetine and Oxybutynin)
- Effects of the combination of atomoxetine and oxybutynin on obstructive sleep apnea endotypic traits. CHEST. doi:10.1016/j.chest.2020.01.012 [MEDLINE]
We recently showed that administration of the combination of the noradrenergic drug atomoxetine plus the antimuscarinic oxybutynin (ato-oxy) prior to sleep greatly reduced OSA severity, likely by increasing upper airway dilator muscle activity during sleep. In patients with OSA who performed the ato-oxy trial with an esophageal pressure catheter to estimate ventilatory drive, the effect of the drug combination (n = 17) and of the single drugs (n = 6) was measured on the endotypic traits over a 1-night administration and compared vs placebo. This study also tested if specific traits were predictors of complete response to treatment (reduction in apnea-hypopnea index [AHI] > 50% and < 10 events/h).
Methods The study was a double-blind, randomized, placebo-controlled trial. The arousal threshold, collapsibility (ventilation at eupneic drive [Vpassive]), ventilation at arousal threshold, and loop gain (LG1), were calculated during spontaneous breathing during sleep. Muscle compensation (upper airway response) was calculated as a function of ventilation at arousal threshold adjusted for Vpassive. Ventilation was expressed as a percentage of the eupneic level of ventilation (%eupnea). Data are presented as mean [95% CI].
Results Compared with placebo, ato-oxy increased Vpassive by 73 [54 to 91]%eupnea (P < .001) and muscle compensation by 29 [8 to 51]%eupnea (P = .012), reduced the arousal threshold by –9 [–14 to –3]% (P = .022) and LG1 by –11 [–22 to 2]% (P = .022). Atomoxetine alone significantly reduced arousal threshold and LG1. Both agents alone improved collapsibility (Vpassive) but not muscle compensation. Patients with lower AHI, higher Vpassive, and higher fraction of hypopneas over total events had a complete response with ato-oxy.
Findings Ato-oxy markedly improved the measures of upper airway collapsibility, increased breathing stability, and slightly reduced the arousal threshold. Patients with relatively lower AHI and less severe upper airway collapsibility had the best chance for OSA resolution with ato-oxy.
Perioperative Management of Obstructive Sleep Apnea (OSA)
Recommendations (American Society of Anesthesiologists Practice Guidelines for the Perioperative Management of Patients with Obstructive Sleep Apnea, 2014) (Anesthesiology, 2014) [MEDLINE]
Preoperative Evaluation
- General Comments
- In Observational Studies, Higher Body Mass Index (BMI) Values are Observed Obstructive Sleep Apnea Patients, as Compared to Non-Obstructive Sleep Apnea Patients
- Similarly, a Higher Frequency of Obstructive Sleep Apnea is Reported in Obese Patients, as Compared to Non-Obese Patients (Category B1-H Evidence)
- Identification/Assessment of Obstructive Sleep Apnea
- Clinical Symptoms/Signs Suggesting Possible Obstructive Sleep Apnea
- Predisposing Physical Characteristics
- Anatomical Nasal Obstruction
- BMI 35 kg/m2 (in Adult) or 95th Percentile for Age/Sex (in Child)
- Craniofacial Abnormalities Affecting the Airway
- Neck Circumference 17 in (Male) or 16 in (Female)
- Tonsils Nearly Touching or Touching in the Midline
- History of Apparent Airway Obstruction During Sleep (≥2 of the Following) (If Patient Lives Alone or Sleep is Not Observed by Another Person, Then Only One Condition Needs to Be Present)
- Awakens from Sleep with Choking Sensation
- Frequent Arousals from Sleep
- Frequent Snoring
- Loud Snoring (Loud Enough to Be Heard Through a Closed Door)
- Observed Pauses in Breathing During Sleep
- Features in Pediatric Patients
- Intermittent vocalization during Sleep
- Parental Report of Restless Sleep, difficulty breathing, or struggling respiratory efforts during sleep
- Child with night terrors
- Child Sleeps in Unusual Positions
- Child with new onset enuresis
- Somnolence (≥1 of the Following)
- Frequent Daytime Somnolence or Fatigue Despite Adequate “Sleep”
- Falls Asleep Easily in a Nonstimulating Environment (Such as Watching Television, Reading, Riding in or Driving a Car) Despite Adequate “Sleep”
- Pediatric Features
- Parent/Teacher Comments that Child Appears Sleepy During the Day, is Easily Distracted, is Overly Aggressive, is Irritable, or Has Difficulty Concentrating
- Child Often Difficult to Arouse at Usual Awakening Time
- Predisposing Physical Characteristics
- If a Patient Has Symptoms/Signs in ≥2 of the Above Categories, There is a Significant Probability That Patient Has Obstructive Sleep Apnea
- Severity of Obstructive Sleep Apnea Maye Be Determined by Sleep Study
- If a Sleep Study is Not Available, Such Patients Should Be Treated as Though They Have Moderate Sleep Apnea Unless ≥1 Symptoms/Signs Above is Severely Abnormal (e.g. Markedly Increased Body Mass Index or Neck Circumference, Respiratory Pauses Which are Frightening to the Observer, Patient Regularly Falls Asleep within Minutes After Being Left Unstimulated without Another Explanation) in Which Case They Should Be Treated as Though They Have Severe Obstructive Sleep Apnea
- If a Sleep Study Has Been Previously Performed, the Results Should Be Used to Determine the Patient’s Perioperative Anesthetic Management
- However, Because Sleep Laboratories Differ in Their Criteria for Detecting Episodes of Apnea and Hypopnea, the the Sleep Laboratory’s Assessment (None, Mild, Moderate, or Severe) Should Take Precedence Over the Actual Apnea-Hypopnea Index
- If the Overall Severity of Obstructive Sleep Apnea is Not Indicated, it May Be Determined by Using the Following
- Adult AHI 0-5: none
- Adult AHI 6-20: mild
- Adult AHI 21-40: moderate
- Adult AHI >40: severe
- Clinical Symptoms/Signs Suggesting Possible Obstructive Sleep Apnea
- Anesthesiologists/Surgeons Should Develop a Protocol Whereby Patients in Whom the Possibility of Obstructive Sleep Apnea is Suspected on Clinical Grounds are Evaluated Long Enough Before the Day of Surgery to Allow Preparation of a Perioperative Management Plan
- Evaluation May Be Initiated in a Preanesthesia Clinic (if Available) or By Direct Consultation from the Surgeon to the Anesthesiologist
- Preoperative Evaluation Should Include Comprehensive Review of Medical Records (if Available), Interview with the Patient/Family, and Physical Examination
- Medical Records Review Should Include Checking for a History of Airway Difficulty with Prior Anesthetics, History of Hypertension or Other Cardiovascular Problems, and History of Other Congenital/Acquired Medical Conditions
- Patient/Family Interview Should Include Questions Related to Snoring, Apnea Episodes, Frequent Sleep Arousals (e.g. Vocalization, Shifting Position, and Extremity Movements), Morning Headaches, and Daytime Somnolence
- Literature is Insufficient to Evaluate the Efficacy of Conducting a Patient/Family Interview to Identify the Presence of Obstructive Sleep Apnea
- Observational Studies Evaluating Screening Protocols/Questionnaires to Identify Adult Obstructive Sleep Apnea Patients Report Sensitivity Values Ranging from 36-86%, Specificity Values Ranging from 31-95%, Positive Predictive Values Ranging from 72-96%, and Negative Predictive Values ranging from 30-82%, Based on Apnea–Hypopnea Index or Respiratory Disturbance Index Scores of ≥5 (Category B2-B Evidence)
- Physical Examination Should Include Evaluation of the Airway, Nasopharyngeal Characteristics, Neck Circumference, Tonsil Size, and Tongue Volume
- Comparative Observational Studies Report Differences in Neck Circumference, Tongue Size, Nasal/Oropharyngeal Airway Structures When Comparing Obstructive Sleep Apnea with Non-Obstructive Sleep Apnea Patients (Category B1-H Evidence)
- Review of Prior Sleep Studies is Encouraged
- If Any Characteristics Noted During Preoperative Evaluation Suggest that the Patient has Obstructive Sleep Apnea, the Anesthesiologist/Surgeon Should Jointly Decide Whether to Manage the Patient Perioperatively Based on Clinical Criteria Alone or to Obtain a Sleep Study, Conduct a More Extensive Airway Examination, and Initiate Indicated Obstructive Sleep Apnea Treatment in Advance of Surgery
- If the Preoperative Evaluation Does Not Occur Until the Day of Surgery, the Surgeon and Anesthesiologist Together May Elect for Presumptive Management Based on Clinical Criteria or a Last-Minute Delay of the Surgery
- For Safety, Clinical Criteria Should Have a High Degree of Sensitivity (Despite the Resulting Low Specificity), Meaning that Some Patients May Be Treated More Aggressively than Would Be Necessary than if a Sleep Study was Available
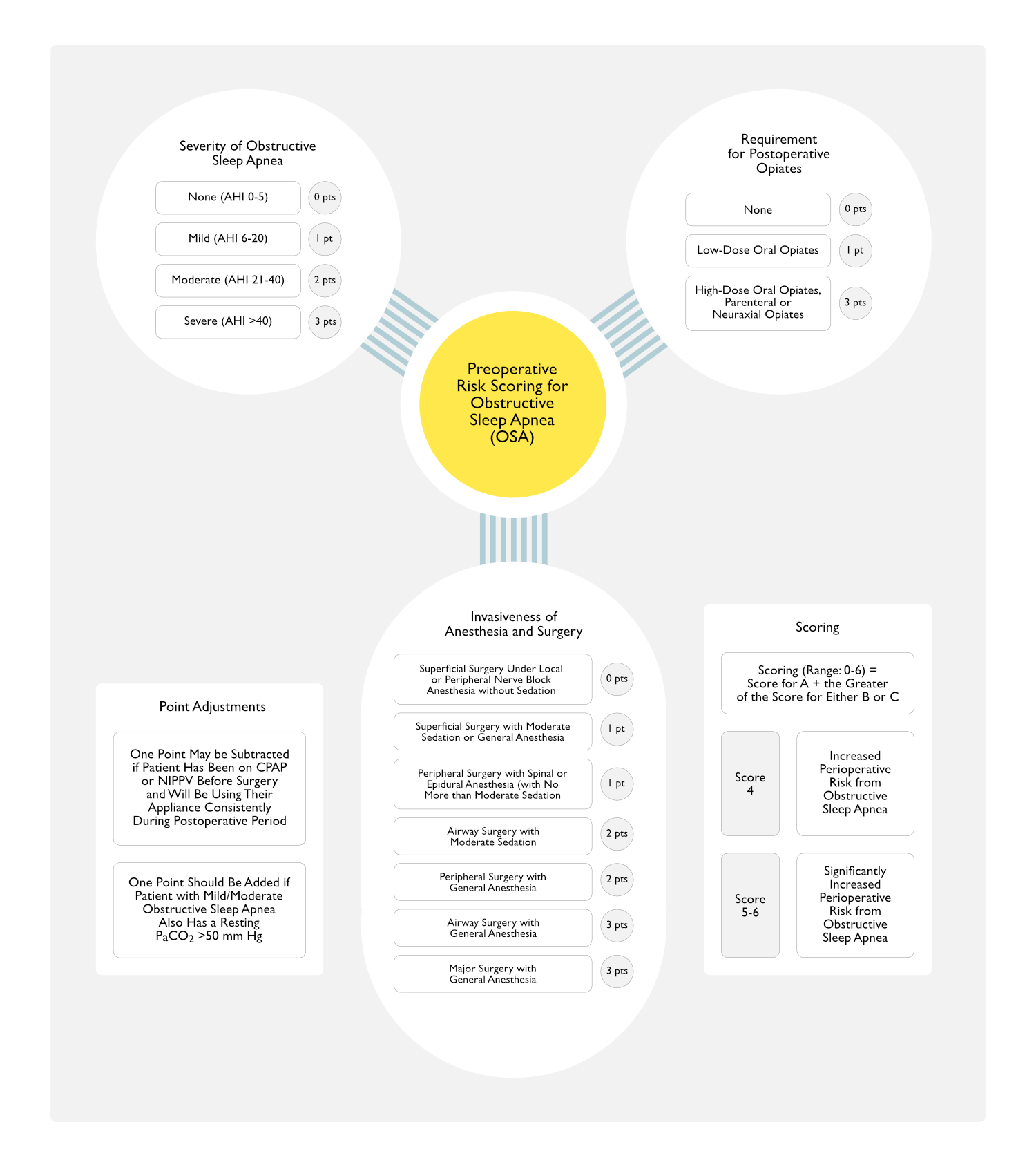
- Severity of the Patient’s Obstructive Sleep Apnea, the Invasiveness of the Diagnostic or Therapeutic Procedure, and the Requirement for Postoperative Analgesics Should Be Considered in Determining Whether a Patient is at Increased Perioperative Risk from Obstructive Sleep Apnea
- Scoring System for Perioperative Risk from Obstructive Sleep Apnea (This Scoring System Has Not Been Validated and is Meant to Be Used Only as a Guide)
- Severity of Obstructive Sleep Apnea Based on Sleep Study (or Clinical Indicators if Sleep Study is Not Available)
- None: 0 pts
- Mild OSA Severity: 1 pt
- Moderate OSA Severity: 2 pts
- Severe OSA Severity: 3 pts
- Invasiveness of Anesthesia and Surgery
- Superficial Surgery Under Local or Peripheral Nerve Block Anesthesia without Sedation: 0 pts
- Superficial Surgery with Moderate Sedation or General Anesthesia: 1 pt
- Peripheral Surgery with Spinal or Epidural Anesthesia (with No More than Moderate Sedation) 1 pt
- Airway Surgery with Moderate Sedation 2
- Peripheral Surgery with General Anesthesia: 2 pts
- Airway Surgery with General Anesthesia: 3 pts
- Major Surgery with General Anesthesia: 3 pts
- Requirement for Postoperative Opiates
- None: 0 pts
- Low-Dose Oral Opiates: 1 pt
- High-Dose Oral Opiates, Parenteral or Neuraxial Opiates: 3 pts
- Scoring (Range: 0-6) = Score for A + the Greater of the Score for Either B or C
- One Point May be Subtracted if a Patient Has Been on CPAP or NIPPV Before Surgery and Will Be Using Their Appliance Consistently During the Postoperative Period
- One Point Should Be Added if a Patient with Mild/Moderate Obstructive Sleep Apnea Also Has a Resting PaCO2 >50 mm Hg
- Patient with Score 4 May Be at Increased Perioperative Risk from Obstructive Sleep Apnea
- Patient with Score of 5-6 May Be at Significantly Increased Perioperative Risk from Obstructive Sleep Apnea
- Severity of Obstructive Sleep Apnea Based on Sleep Study (or Clinical Indicators if Sleep Study is Not Available)
- Scoring System for Perioperative Risk from Obstructive Sleep Apnea (This Scoring System Has Not Been Validated and is Meant to Be Used Only as a Guide)
- Patient/Family and Surgeon Should Be Informed of the Potential Implications of Obstructive Sleep Apnea on the Patient’s Perioperative Course
Inpatient vs Outpatient Surgery
- Before Patients at Increased Perioperative Risk from Obstructive Sleep Apnea are Scheduled to Undergo Surgery, Determination Should Be Made Regarding Whether a Surgical Procedure is Most Appropriately Performed on an Inpatient vs Outpatient Basis
- Factors to Be Considered in Determining Whether Inpatient vs Outpatient Care is Appropriate Include the Following
- Adequacy of Postdischarge Observation
- Anatomical and Physiologic Abnormalities
- Availability of Emergency Difficult Airway Equipment and Respiratory Care Equipment
- Capabilities of the Outpatient Facility
- Clinical Laboratory Facilities
- Nature of Surgery
- Need for Postoperative Opiates
- Patient Age
- Presence of Transfer Agreement with an Inpatient Facility
- Radiology Facilities
- Sleep Apnea Status
- Status of Coexisting Diseases
- Type of Anesthesia
- Factors to Be Considered in Determining Whether Inpatient vs Outpatient Care is Appropriate Include the Following
Preoperative Preparation
- Preoperative Initiation of Continuous Positive Airway Pressure (CPAP) Should Be Considered, Particularly if Obstructive Sleep Apnea is Severe
- For Patients Who Do Not Respond Adequately to CPAP, Noninvasive Positive Pressure Ventilation Should Be Considered
- Literature is Insufficient to Evaluate the Impact of the Preoperative Use of NIPPV
- Clinical Efficacy
- An Observational Study Reported Lower Frequency of Serious Postoperative Complications (i.e. Cardiac Events, Complications Needing Intensive Care Unit Transfer or Urgent Respiratory Support) When Preoperative At-Home CPAP is Compared with No Preoperative CPAP (Category B1-B Evidence) (Mayo Clin Proc, 2001) [MEDLINE]
- Preoperative Diagnosis of Obstructive Sleep Apnea and Use of CPAP Therapy Decrease the Risks of Postoperative Pulmonary and Cardiovascular Complications (Sleep Med, 2022) [MEDLINE]: n = 46 studies
- Subgroup Analysis Indicated that Preoperative Diagnosis and the Use of CPAP Therapy Decrease the Risk of Postoperative Respiratory Complications (Odds Ratio = 1.87; 95% CI: 1.43-2.43) and Cardiac Complications (Odds Ratio = 1.17; 95% CI: 0.91-1.51)
- Literature is Insufficient to Evaluate the Efficacy of Preoperative Weight Loss
- For Patients Who Do Not Respond Adequately to CPAP, Noninvasive Positive Pressure Ventilation Should Be Considered
- Preoperative Use of Mandibular Advancement Devices or Oral Appliances and Preoperative Weight Loss Should Be Considered When Feasible
- A Patient Who Has Had Corrective Airway Surgery (Such as Uvulopalatopharyngoplasty or Surgical Mandibular Advancement) Should Be Assumed to Remain at Risk of Obstructive Sleep Apnea Complications Unless a Normal Sleep Study Has Been Obtained and Clinical Symptoms Have Not Returned
- Patients with Known or Suspected Obstructive Sleep Apnea May Have Difficult Airways and Therefore Should Be Managed According to the American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway
Intraoperative Management
- Because of Their Propensity for Airway Collapse and Sleep Deprivation, Patients at Increased Perioperative Risk from Obstructive Sleep Apnea are Especially Susceptible to the Respiratory Depressant and Airway Effects of Sedatives, Opiates, and Inhaled Anesthetics
- Therefore, the Potential for Postoperative Respiratory Compromise Should Be Considered in Selecting Intraoperative Medications
- For Superficial Procedures, Consider the Use of Local Anesthesia or Peripheral Nerve Blocks (with or without Moderate Sedation)
- If Moderate Sedation is Used, Ventilation Should Be Continuously Monitored by Capnography or Another Automated Method (if Feasible) Because of the Increased Risk of Undetected Airway Obstruction in These Patients
- Consider Administering CPAP or Using an Oral Appliance During Sedation to Patients Previously Treated with These Modalities
- General Anesthesia with a Secure Airway is Preferable to Deep Sedation without a secure airway, Particularly for Procedures Which May Mechanically Compromise the Airway
- Major Conduction Anesthesia (Spinal/Epidural) Should Be Considered for Peripheral Procedures
- Unless There is a Medical/Surgical Contraindication, Patients at Increased Perioperative Risk from Obstructive Sleep Apnea Should Be Extubated While Awake
- Full Reversal of Neuromuscular Block Should Be Verified Before Extubation
- When Possible, Extubation and Recovery Should Be Performed in the Lateral, Semiupright, or Other Nonsupine Position
Postoperative Management
- Regional Analgesic Techniques Should Be Considered to Decrease/Eliminate the Requirement for Systemic Opiates in Patients at Increased Perioperative Risk from Obstructive Sleep Apnea
- If Neuraxial Analgesia is Planned, Weigh the Benefits (Improved Analgesia, Decreased Requirement for Systemic Opiates) and Risks (Respiratory Depression from Rostral Spread) of Using an Opiate or Opiate–Local Anesthetic Mixture Rather than a Local Anesthetic Alone
- If Patient-Controlled Systemic Opiates are Utilized, Continuous Background Infusions Should Be Avoided or Utilized with Extreme Caution
- To Decrease Opiate Requirements, Nonsteroidal Anti-Inflammatory Agents and Other Modalities (Ice, Transcutaneous Electrical Nerve Stimulation) Should Be Considered (If Appropriate)
- Concurrent Administration of Sedative Agents (Benzodiazepines and Barbiturates) Increases the Risk of Respiratory Depression and Airway Obstruction
- Supplemental Oxygen Should Be Administered Continuously to All Patients Who are at Increased Perioperative Risk from Obstructive Sleep Apena Until They are Able to Maintain Their Baseline Oxygen Saturation While Breathing Room Air
- Note that the Use of Supplemental Oxygen May Increase the Duration of Apneic Episodes and May Hinder Detection of Atelectasis, Transient Apnea, and Hypoventilation by Pulse Oximetry
- When Feasible, CPAP or Noninvasive Positive-Pressure Ventilation (with/without Supplemental Oxygen) Should Be Continuously Administered to Patients Who were Using these Modalities Preoperatively (Unless Contraindicated by the Surgical Procedure)
- Compliance with CPAP or Noninvasive Positive-Pressure Ventilation May Be Improved if Patients Bring Their Own Equipment to the Hospital
- If Possible, Patients at Increased Perioperative Risk from Obstructive Sleep Apnea Should Be Placed in the Nonsupine Position throughout the Recovery Process
- Hospitalized Patients Who are at Increased Risk of Respiratory Compromise from Obstructive Sleep Apnea Should Have Continuous Pulse Oximetry Monitoring After Discharge from the Recovery Room
- Continuous Monitoring May Be Provided in a Critical Care or Stepdown Unit, by Telemetry on a Hospital Ward, or By a Dedicated, Appropriately Trained Professional Observer in the Patient’s Room
- Continuous Monitoring Should Be Maintained as Long as the Patient Remains at Increased Risk
- If Frequent or Severe Airway Obstruction or Hypoxemia Occurs During Postoperative Monitoring, Initiation of Nasal CPAP or Noninvasive Positive-Pressure Ventilation Should Be Considered
Criteria for Discharge to Unmonitored Settings
- Patients at Increased Perioperative Risk from OSA Should Not Be Discharged from the Recovery Area to an Unmonitored Setting (i.e. Home or Unmonitored Hospital Bed) Until They are No Longer at Risk for Postoperative Respiratory Depression
- Because of Their Propensity to Develop Airway Obstruction or Central Respiratory Depression, This May Require a Longer Stay as Compared with Non-OSA Patients Undergoing Similar Procedures
- To Establish that Patients are Able to Maintain Adequate Oxygen Saturation Levels While Breathing Room Air, Respiratory Function May Be Determined by Observing Patients in an Unstimulated Environment, Preferably While Asleep
Prognosis
- Obstructive Sleep Apnea Increases Mortality Rate (Chest, 1988) [MEDLINE]
- Patients with an Average of >20 Apneas/hr were Found to Have an 8-yr Cumulative Mortality of 37%, as Compared with 4% in Those with an index <20 Apneas/hr
- Wisconsin Sleep Cohort Study (Sleep, 2008) [MEDLINE]
- Untreated Sleep-Disordered Breathing Increases Mortality, Independent of Age/Sex/BMI
- Results Were Similar Even After Accounting for Symptoms of Daytime Sleepiness
- Busselton Health Study (Sleep, 2008) [MEDLINE]
- Moderate-Severe OSA is Associated with Increased All-Cause Mortality
- Sleep Heart Health Study (PLoS Med, 2009) [MEDLINE]
- Sleep-Disordered Breathing Increased All-Cause Mortality (and Specifically that Due to Coronary Artery Disease), Particularly in Males age 40-70
- Database Study (Otolaryngol Head Neck Surg, 2012) [MEDLINE]: increased OSA severity (quantified by AHI/apnea index/desaturation index) is independently associated with all-cause mortality in patients <50 y/o (after adjustment for confounding factors)
References
General
- Mortality and apnea index in obstructive sleep apnea: experiences in 385 male patients. Chest. 1988;94:9-14 [MEDLINE]
- The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993; 328:1230-5 [MEDLINE]
- Postoperative complications in patients with obstructive sleep apnea syndrome undergoing hip or knee replacement: a case-control study. Mayo Clin Proc. 2001;76:897-905 [MEDLINE]
- Portable Monitoring Task Force of the American Academy of Sleep Medicine. Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnea in adult patients. J Clin Sleep Med 2007;3(7):737-747 [MEDLINE]
- A systemic review of obstructive sleep apnea and its implications for anesthesiologists. Anesth Analg. 2008;107:1543-63 [MEDLINE]
- Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin Sleep Cohort. Sleep. 2008;31:1071-8 [MEDLINE]
- Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med. 2009;6:e1000132 [MEDLINE]
- Prevalence of undiagnosed obstructive sleep apnea among adult surgical patients in an academic medical center. Sleep Med. 2009;10:753-8 [MEDLINE]
- Are sleep studies appropriately done in the home? Respir Care 2010;55(1):66-75 [MEDLINE]
- Obstructive sleep apnea-hypopnea and incident stroke: the sleep heart health study. Am J Respir Crit Care Med. 2010 Jul 15;182(2):269-77. doi: 10.1164/rccm.200911-1746OC. Epub 2010 Mar 25 [MEDLINE]
- A prospective polysomnographic study on the evolution of complex sleep apnoea. Eur Respir J 2011;38(2):329-337 [MEDLINE]
- Assessing sleepiness and sleep disorders in Australian long-distance commercial vehicle drivers: self-report versus an “at home” monitoring device. Sleep 2012;35:469-475 [MEDLINE]
- Obstructive sleep apnea is associated with fatty liver and abnormal liver enzymes: a meta-analysis. Obes Surg 2013;23(11): 1815-1825 [MEDLINE]
- Nonalcoholic fatty liver disease, nocturnal hypoxia, and endothelial function in patients with sleep apnea. Chest 2014;145(3):525-533 [MEDLINE]
- Risk of obstructive sleep apnea with daytime sleepiness is associated with liver damage in non-morbidly obese patients with nonalcoholic fatty liver disease. PLoS One 2014;9(4):e96349 [MEDLINE]
- Diagnosis of obstructive sleep apnea in adults: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med 2014;161:210-220 [MEDLINE]
- International classification of sleep disorders-third edition: highlights and modifications. Chest. 2014 Nov;146(5):1387-94. doi: 10.1378/chest.14-0970 [MEDLINE]
- Sleep apnea related risk of motor vehicle accidents is reduced by continuous positive airway pressure: Swedish Traffic Accident Registry Data. Sleep 2015;38:341-349 [MEDLINE]
Risk Factors/Clinical Predictors
- Smoking as a risk factor for sleep-disordered breathing. Arch Intern Med. 1994 Oct 10;154(19):2219-24 [MEDLINE]
Clinical
- Perioperative complications and risk factors in the surgical treatment of obstructive sleep apnea syndrome. Laryngoscope. 1989;99(11):1125 [MEDLINE]
- Postoperative obstructive sleep apnoea. Haemodynamic effects of treatment with nasal CPAP. Anaesthesia. 1991;46(10):849 [MEDLINE]
- Nasal continuous positive airway pressure in the perioperative management of patients with obstructive sleep apnea submitted to surgery. Chest. 1995;107(2):367 [MEDLINE]
- Three sudden postoperative respiratory arrests associated with epidural opioids in patients with sleep apnea. Anesth Analg. 1997;85(2):452 [MEDLINE]
- Relationship between difficult tracheal intubation and obstructive sleep apnoea. Br J Anaesth. 1998;80(5):606 [MEDLINE]
- Postoperative complications in patients with obstructive sleep apnea syndrome undergoing hip or knee replacement: a case-control study. Mayo Clin Proc. 2001 Sep;76(9):897-905. doi: 10.4065/76.9.897 [MEDLINE]
- Postoperative complications in patients with obstructive sleep apnea syndrome undergoing hip or knee replacement: a case-control study. Mayo Clin Proc. 2001;76(9):897 [MEDLINE]
- Difficult endotracheal intubation in patients with sleep apnea syndrome. Anesth Analg. 2002;95(4):1098 [MEDLINE]
- Upper airway management of the adult patient with obstructive sleep apnea in the perioperative period–avoiding complications. Sleep. 2003;26(8):1060 [MEDLINE]
- Upper airway management of the adult patient with obstructive sleep apnea in the perioperative period–avoiding complications. Sleep. 2003;26(8):1060 [MEDLINE]
- Predictors of difficult airway management in morbid obesity patients. Eur J Anaesthesiol. 2006;23:263
- A systemic review of obstructive sleep apnea and its implications for anesthesiologists. Anesth Analg. 2008 Nov;107(5):1543-63. doi: 10.1213/ane.0b013e318187c83a [MEDLINE]
- Perioperative pulmonary outcomes in patients with sleep apnea after noncardiac surgery. Anesth Analg. 2011 Jan;112(1):113-21 [MEDLINE]
- Obstructive sleep apnoea and perioperative complications in bariatric patients. Br J Anaesth. 2011;106(1):131 [MEDLINE]
- Obesity as a risk factor for sedation-related complications during propofol-mediated sedation for advanced endoscopic procedures. Gastrointest Endosc. 2011;74(6):1238 [MEDLINE]
- Postoperative complications in patients with obstructive sleep apnea. Chest. 2012;141(2):436 [MEDLINE]
- Obstructive sleep apnea as a risk factor for postoperative complications after revision joint arthroplasty. J Arthroplasty. 2012 Sep;27(8 Suppl):95-8 [MEDLINE]
- Meta-analysis of the association between obstructive sleep apnoea and postoperative outcome. Br J Anaesth. 2012 Dec;109(6):897-906 [MEDLINE]
- Obstructive sleep apnea and incidence of postoperative delirium after elective knee replacement in the nondemented elderly. Anesthesiology. 2012 Apr;116(4):788-96 [MEDLINE]
- Sleep-disordered breathing and postoperative outcomes after elective surgery: analysis of the nationwide inpatient sample. Chest. 2013 Sep;144(3):903-14 [MEDLINE]
- Sleep-disordered breathing and postoperative outcomes after bariatric surgery: analysis of the nationwide inpatient sample. Obes Surg. 2013 Nov;23(11):1842-51 [MEDLINE]
- Obstructive sleep apnea screening and postoperative mortality in a large surgical cohort. Sleep Med. 2013 May;14(5):407-15 [MEDLINE]
- A matched cohort study of postoperative outcomes in obstructive sleep apnea: could preoperative diagnosis and treatment prevent complications? Anesthesiology. 2014;121(4):707 [MEDLINE]
- Comparing ease of intubation in obese and lean patients using intubation difficulty scale. Anesth Essays Res. 2014;8(2):168 [MEDLINE]
- Practice guidelines for the perioperative management of patients with obstructive sleep apnea: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Management of patients with obstructive sleep apnea. Anesthesiology. 2014 Feb;120(2):268-86 [MEDLINE]
- The Impact of Untreated Obstructive Sleep Apnea on Cardiopulmonary Complications in General and Vascular Surgery: A Cohort Study. Sleep. 2015;38(8):1205 [MEDLINE]
- Does Obstructive Sleep Apnea Influence Perioperative Outcome? A Qualitative Systematic Review for the Society of Anesthesia and Sleep Medicine Task Force on Preoperative Preparation of Patients with Sleep-Disordered Breathing. Anesth Analg. 2016;122(5):1321 [MEDLINE]
- Sedation Challenges: Obesity and Sleep Apnea. Gastrointest Endosc Clin N Am. 2016;26(3):527 [MEDLINE]
- Postoperative Complications in Patients With Unrecognized Obesity Hypoventilation Syndrome Undergoing Elective Noncardiac Surgery. Chest. 2016;149(1):84 [MEDLINE]
- Obesity hypoventilation syndrome, sleep apnea, overlap syndrome: perioperative management to prevent complications. Curr Opin Anaesthesiol. 2017;30(1):146 [MEDLINE]
- Preoperatively Screened Obstructive Sleep Apnea Is Associated With Worse Postoperative Outcomes Than Previously Diagnosed Obstructive Sleep Apnea. Anesth Analg. 2017;125(2):593 [MEDLINE]
- Sleep-Disordered Breathing, Postoperative Delirium, and Cognitive Impairment. Anesth Analg. 2017;124(5):1626 [MEDLINE]
- Patients at High Risk for Obstructive Sleep Apnea Are at Increased Risk for Atrial Fibrillation After Cardiac Surgery: A Cohort Analysis. Anesth Analg. 2018;126(6):2025 [MEDLINE]
- Is obstructive sleep apnea associated with difficult airway? Evidence from a systematic review and meta-analysis of prospective and retrospective cohort studies. PLoS One. 2018;13(10):e0204904 [MEDLINE]
- Association of Unrecognized Obstructive Sleep Apnea With Postoperative Cardiovascular Events in Patients Undergoing Major Noncardiac Surgery. JAMA. 2019;321(18):1788 [MEDLINE]
- Association of Unrecognized Obstructive Sleep Apnea With Postoperative Cardiovascular Events in Patients Undergoing Major Noncardiac Surgery. JAMA. 2019;321(18):1788 [MEDLINE]
- The relationship between obstructive sleep apnoea and postoperative delirium and pain: an observational study of a surgical cohort. Anaesthesia. 2019;74(12):1542 [MEDLINE]
- Association of obstructive sleep apnea and postoperative cardiac complications: A systematic review and meta-analysis with trial sequential analysis. J Clin Anesth. 2020;62:109731 [MEDLINE]
- Risk of major cardiovascular and cerebrovascular complications after elective surgery in patients with sleep-disordered breathing: A retrospective cohort analysis. Eur J Anaesthesiol. 2020;37(8):688 [MEDLINE]
- Association of obstructive sleep apnea and postoperative cardiac complications: A systematic review and meta-analysis with trial sequential analysis. J Clin Anesth. 2020;62:109731 [MEDLINE]
- Differential Perioperative Outcomes in Patients With Obstructive Sleep Apnea, Obesity, or a Combination of Both Undergoing Open Colectomy: A Population-Based Observational Study. Anesth Analg. 2021;133(3):755 [MEDLINE]
- Association of Obstructive Sleep Apnea With Difficult Intubation: Prospective Multicenter Observational Cohort Study. Anesth Analg. 2021;133(1):196 [MEDLINE]
- Meta-analysis of the association between obstructive sleep apnea and postoperative complications. Sleep Med. 2022;91:1 [MEDLINE]
- Review of the prevalence, pathogenesis and management of OSA-COPD overlap. Sleep Breath. 2022 Dec;26(4):1551-1560. doi: 10.1007/s11325-021-02540-8 [MEDLINE]
Treatment
Weight Loss
- Multimodal telemonitoring for weight reduction in sleep apnea patients: A randomized controlled trial. Chest. 2022 Aug 20;S0012-3692(22)03651-0. doi: 10.1016/j.chest.2022.07.032 [MEDLINE]
CPAP
- Practice parameters for the use of autotitrating continuous positive airway pressure devices for titrating pressures and treating adult patients with obstructive sleep apnea syndrome: an update for 2007. An American Academy of Sleep Medicine report. Sleep 2008;31(1): 141-147 [MEDLINE]
- Clinical guidelines for the manual titration of positive airway pressure in patients with obstructive sleep apnea. J Clin Sleep Med. 2008 Apr 15;4(2):157-71 [MEDLINE]
- Portable monitoring and autotitration vs polysomnography for the diagnosis and treatment of sleep apnea. Sleep 2008;31(10):1423-1431 [MEDLINE]
- Effects of a short course of eszopiclone on continuous positive airway pressure adherence: a randomized trial. Ann Intern Med. 2009 Nov 17;151(10):696-702. doi: 10.7326/0003-4819-151-10-200911170-00006 [MEDLINE]
- A systematic review of CPAP adherence across age groups: Clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev 2011;15(6):343-356 [MEDLINE]
- Air leak is associated with poor adherence to autoPAP therapy. Sleep. 2011 Jun 1;34(6):801-6. doi: 10.5665/SLEEP.1054 [MEDLINE]
- Residual sleep-disordered breathing during autotitrating continuous positive airway pressure therapy. Eur Respir J 2012;39(6): 1391-1397 [MEDLINE]
- Cardiometabolic changes after continuous positive airway pressure for obstructive sleep apnoea: a randomised sham-controlled study. Thorax 2012;67:1081-1089 [MEDLINE]
- The effect of continuous positive airway pressure treatment on blood pressure: a systematic review and meta-analysis of randomized controlled trials. J Clin Sleep Med 2012;8:587-596 [MEDLINE]
- The impact of posttraumatic stress disorder on CPAP adherence in patients with obstructive sleep apnea. J Clin Sleep Med 2012;8(6):667-72. doi: 10.5664/jcsm.2260 [MEDLINE]
- Health Outcomes of Continuous Positive Airway Pressure versus Oral Appliance Treatment for Obstructive Sleep Apnea. Am J Respir Crit Care Med. 2013 Apr 15;187(8):879-87 [MEDLINE]
- The effect of continuous positive air pressure (CPAP) on nightmares in patients with posttraumatic stress disorder (PTSD) and obstructive sleep apnea (OSA). J Clin Sleep Med 2014;10(6):631-636. doi: 10.5664/jcsm.3786 [MEDLINE]
- Sleep apnea related risk of motor vehicle accidents is reduced by continuous positive airway pressure: Swedish Traffic Accident Registry Data. Sleep 2015;38:341-349 [MEDLINE]
- Continuous positive airway pressure versus standard care for the treatment of people with mild obstructive sleep apnoea (MERGE): a multicentre, randomised controlled trial. Lancet Respir Med. 2020 Apr;8(4):349-358. doi: 10.1016/S2213-2600(19)30402-3 [MEDLINE]
- Effect of obstructive sleep apnoea and its treatment with continuous positive airway pressure on the prevalence of cardiovascular events in patients with acute coronary syndrome (ISAACC study): a randomised controlled trial. Lancet Respir Med. 2020 Apr;8(4):359-367. doi: 10.1016/S2213-2600(19)30271-1 [MEDLINE]
- Air Pollution and the Effectiveness of Positive Airway Pressure Therapy in Individuals with Sleep Apnea: A Retrospective Community-Based Repeated Measures Longitudinal Study. Chest. 2022 Aug 5;S0012-3692(22)01347-2. doi: 10.1016/j.chest.2022.07.017 [MEDLINE]
Adaptive Servo Ventilation
- Efficacy of adaptive servoventilation in treatment of complex and central sleep apnea syndromes. Chest. 2007;132:1839–1846 [MEDLINE]
- Adaptive servoventilation improves cardiac function and respiratory stability. Clin Res Cardiol. 2011;100:107–115 [MEDLINE]
- A prospective polysomnographic study on the evolution of complex sleep apnoea. Eur Respir J 2011;38(2):329-337 [MEDLINE]
- Therapy for sleep hypoventilation and central apnea syndromes. Curr Treat Options Neurol 2012;14(5):427-437 [MEDLINE]
- Adaptive servoventilation for treatment of sleep-disordered breathing in heart failure: a systematic review and meta-analysis. Chest. 2012;142:1211–1221 [MEDLINE]
- Air leak during CPAP titration as a risk factor for central apnea. J Clin Sleep Med 2013;9(11):1187-1191 [MEDLINE]
- The complex sleep apnea resolution study: a prospective randomized controlled trial of continuous positive airway pressure versus adaptive servoventilation therapy. Sleep. 2014 May;37(5):927-34 [MEDLINE]
- SERVE-HF Trial. Adaptive servo-ventilation for central sleep apnea in systolic heart failure. N Engl J Med 2015;373:1095-1105 [MEDLINE]
Mandibular Advancement Device
- Health Outcomes of Continuous Positive Airway Pressure versus Oral Appliance Treatment for Obstructive Sleep Apnea. Am J Respir Crit Care Med. 2013 Apr 15;187(8):879-87 [MEDLINE]
Implantable Upper Airway Stimulation Device
- Treating obstructive sleep apnea with hypoglossal nerve stimulation. Sleep 2011;34(11):1479-1486. doi: 10.5665/sleep.1380 [MEDLINE]
- Implanted upper airway stimulation device for obstructive sleep apnea. Laryngoscope. 2012 Jul;122(7):1626-33. doi: 10.1002/lary.23301. Epub 2012 May 1 [MEDLINE]
- Acute upper airway responses to hypoglossal nerve stimulation during sleep in obstructive sleep apnea. Am J Respir Crit Care Med. 2012 Feb 15;185(4):420-6. doi: 10.1164/rccm.201109-1614OC. Epub 2011 Dec 1 [MEDLINE]
- Evaluation of drug-induced sleep endoscopy as a patient selection tool for implanted upper airway stimulation for obstructive sleep apnea. J Clin Sleep Med. 2013 May 15;9(5):433-8. doi: 10.5664/jcsm.2658 [MEDLINE]
- STAR Trial Group. Upper-airway stimulation for obstructive sleep apnea. N Engl J Med 2014;370:139-149 [MEDLINE]
- Randomized controlled withdrawal study of upper airway stimulation on OSA: short- and long-term effect. Otolaryngol Head Neck Surg 2014;151:880-887 [MEDLINE]
Atomoxetine and Oxybutynin (see Atomoxetine and Oxybutynin)
- XXXX
Perioperative Management of Obstructive Sleep Apnea
- Postoperative complications in patients with obstructive sleep apnea syndrome undergoing hip or knee replacement: A case-control study. Mayo Clin Proc 2001; 76:897–905 [MEDLINE]
- Practice guidelines for the perioperative management of patients with obstructive sleep apnea: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Management of patients with obstructive sleep apnea. Anesthesiology. 2014 Feb;120(2):268-86. doi: 10.1097/ALN.0000000000000053 [MEDLINE]
Prognosis
- Sleep disordered breathing and mortality: 18-year follow-up of the Wisconsin sleep cohort. Sleep 2008;31:1071-1078 [MEDLINE]
- Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep 2008;31:1079-1085 [MEDLINE]
- Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med 2009;6:1-9 [MEDLINE]
- All-cause mortality and obstructive sleep apnea severity revisited. Otolaryngol Head Neck Surg 2012;Epub ahead of print Jun 11 2012 [MEDLINE]
